Characterised by transient sequential colour changesof white, blue and red usually in the fingers and/or toes triggered by cold or emotion. The digits are most commonly affected but Raynaud’s can affect the nose, tongue or nipples. Raynaud’s is classified into primary and secondary subtypes.

Raynaud’s does not cause a fixed discolouration. If this is observed, it suggests another underlying cause such as:
• Peripheral vascular disease
• Embolism
• Adverse effect of drug or chemical exposure: beta-blockers, vinyl chloride cocaine use, interferon, anti-cancer drugs, bromocriptine, ciclosporin, combined oral contraceptives, clonidine
Primary Raynaud’s phenomenon
- Very common and estimated to affect about 10% of women in the UK.
- Typical onset in teenage years or early adulthood
- Rarely presents for the first time above the age of 40 years.
- Occurs with exposure to cold or emotional stress.
- Usually, bilateral
- No ulceration or tissue necrosis
Secondary Raynaud’s phenomenon
- Usually more severe than primary Raynaud’s
- Typically associated with a connective tissue disease
- Can be associated with digital ulcers and necrosis
M.A & S.R/H.B. 25-01-24
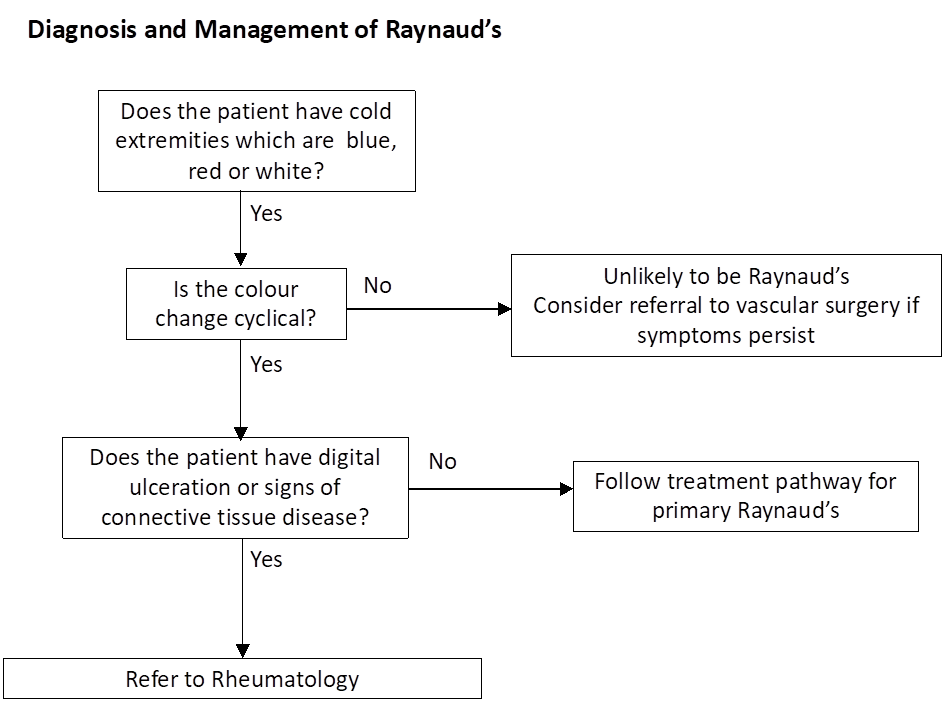
Almost all patients with Raynaud’s can be managed in Primary Care but rheumatology referral should be considered in those with digital ulceration and those suspected to have connective tissue disease. Please refer to the diagnostic algorithm below.
Lifestyle advice
Lifestyle measures should be tried first:
- Keep the whole body warm by wearing layers of clothes, thermal underwear sheep skin gloves and boots and using hand warmers.
- Stop smoking and avoid second-hand smoke. Regular smokers are sensitized to the vasoconstrictive properties of nicotine.
- Avoid cold exposure and changes in temperature where possible, especially sudden changes such as walking into the frozen food section of a grocery store.
- Help terminate an attack by rubbing the hands together, placing the hands under warm water or in a warm place such as the axilla, or rotating the arms in a windmill pattern.
- Avoid medication and other exposures which may provoke Raynaud’s, such as decongestants, methylphenidate, sumatriptan, beta-blockers and caffeine.
- Control or limit emotional stress and anxiety.
Drug treatments
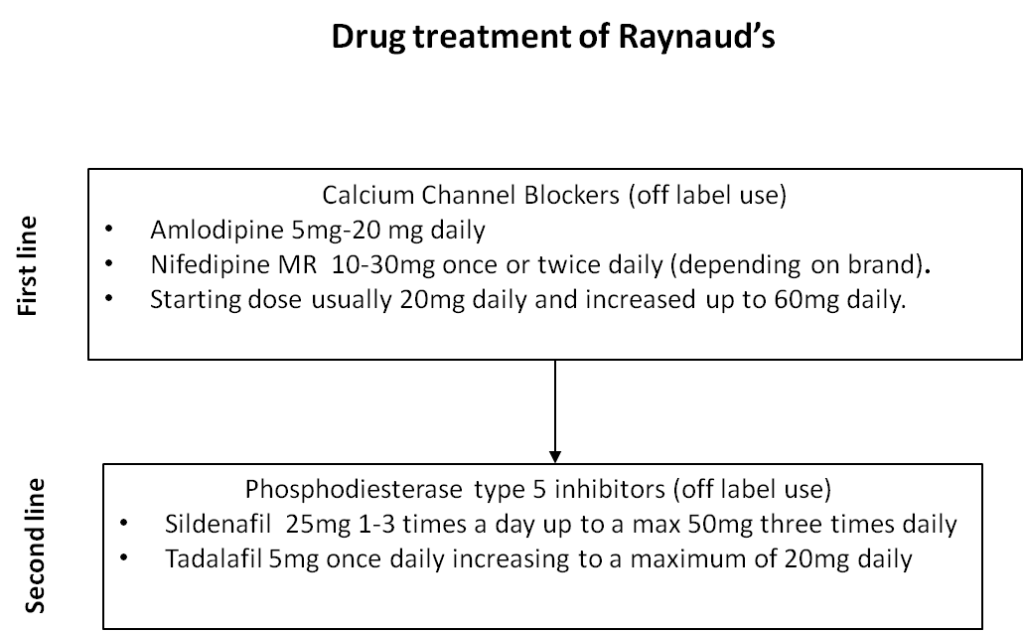
Drug treatments have limited effectiveness in Raynaud’s and often cause adverse effects such as headaches, related to general vasodilatation. No licensed treatments are available for Raynaud’s that can be prescribed in primary care. Calcium antagonists can be tried as first line, followed by PDE-5 inhibitors if calcium antagonists are ineffective or cause adverse effects (see Figure below). Additional treatments which have been tried in Raynaud’s include aspirin, fluoxetine, and statins but the evidence base for the use of these drugs is limited.
Patient information
Scleroderma and Raynaud’s UK – https://www.sruk.co.uk/raynauds/
Raynaud’s Phenomen – Arthritis Research UK – https://www.versusarthritis.org/about-arthritis/conditions/raynauds-phenomenon/













