Information
Gynaecologists with a specialist interest in vulval disorders are available at SJH/RIE. We are able to refer on to Dermatologists, Plastic Surgeons and Gastroenterologists (vulval Crohn’s disease) etc. Every quarter there is a Scottish Vulval Multidisciplinary meeting which we can refer patients to, and attend, to discuss cases that require more specialised/personalised treatment.
Who can refer:
Primary and Secondary Care clinicians
Who to refer:
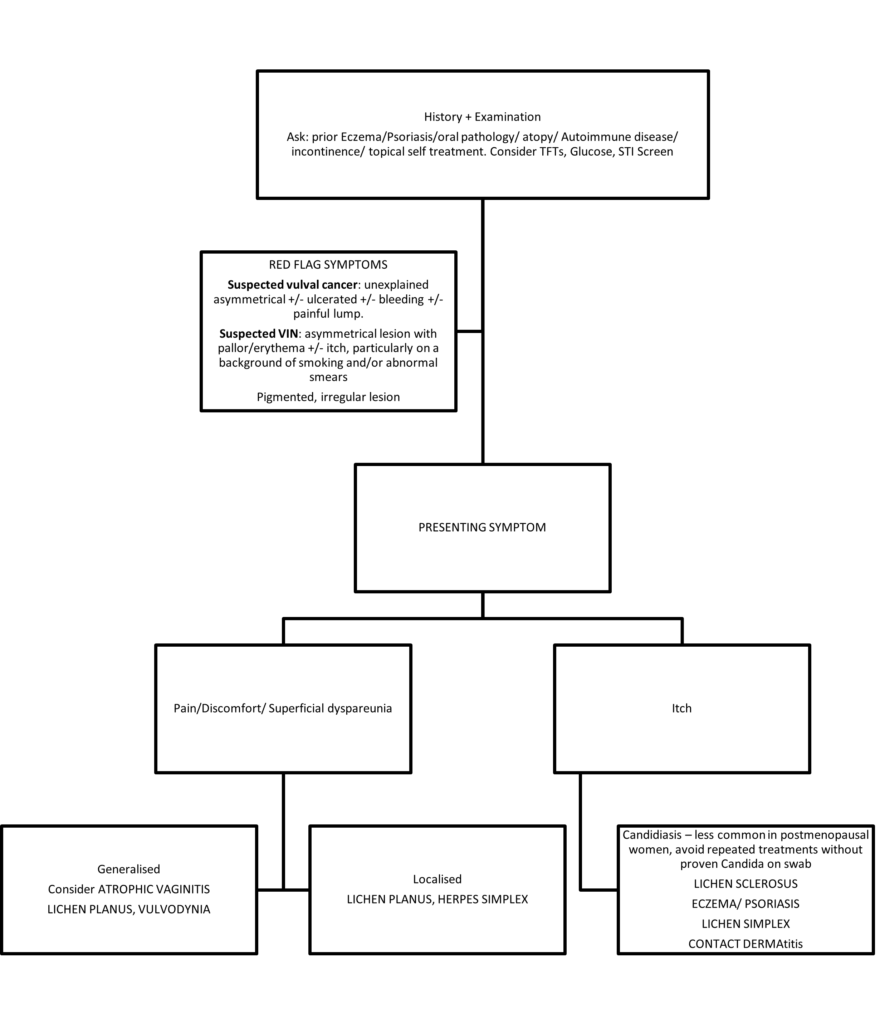
Women with red flag symptoms:
Suspected Vulval Cancer: unexplained asymmetrical / ulcerated/bleeding / painful lumps.
Suspected VIN: asymmetrical lesion with pallor/erythema +/- itch, particularly on a background of smoking and/or abnormal smears.
Pigmented, irregular lesion.
Unresponsive to treatment after at least 6-8 wks
Women with Dermatoses where Primary Care management has been unsuccessful e.g. Lichen Sclerosus, Lichen Planus
History and Examination
Enquire about past history of skin disorders (Eczema, Psoriasis, mouth ulcers), Atopy, Autoimmune Conditions (e.g. thyroid disease, pernicious anaemia).
Investigations
Consider FBC (exclude anaemia), TFTs, blood glucose, STI screen.
Main Presenting Symptom:
Pain/discomfort/superficial dyspareunia
- Generalised: Consider ATROPHIC VAGINITIS, LICHEN PLANUS, VULVODYNIA
- Localised: LICHEN PLANUS, HERPES SIMPLEX Genital herpes images | DermNet (dermnetnz.org)
Itching
Candidiasis – less common in postmenopausal women, avoid repeated treatments without proven Candida on swab
LICHEN SCLEROSUS Vulval lichen sclerosus images | DermNet (dermnetnz.org)
ECZEMA/ PSORIASIS Genital psoriasis images | DermNet (dermnetnz.org)
LICHEN SIMPLEX
CONTACT DERMATITIS
· STI screening should be considered in all patients and vulvovaginal candidiasis Vulvovaginal candidiasis images | DermNet (dermnetnz.org) excluded if the patient presents with vulval itch.
GENERAL ADVICE (for all conditions)
Most women with a vulval disorder will benefit from advice on general care of the vulval skin and avoiding potential irritants.
• Avoid soaps, shower gel, scrubs, bubble baths, deodorants, baby wipes or douches in the vulval area.
• Washing with water only causes dry skin and makes itching worse. Use a soap substitute to clean the vulval area. Use a small amount of the ointment with water to wash skin. This prevents the skin from becoming dry and irritated as it would if soap or water alone was used. The cream/ointment is safe to use frequently.
Formulary | Lothian Joint Formulary (nhs.scot)
• Shower rather than bath if possible and clean the vulval area only once a day. Over cleaning can aggravate vulval symptoms.
• Avoid using sponges or flannels to wash the vulva which can irritate the skin. Wash vulva with a soap substitute with a hand. Gently dab the vulval area dry with a soft towel or use a hairdryer on a cool setting held well away from the skin.
• Wear loose-fitting silk or cotton underwear. Tight-fitting clothes such as tights, cycling shorts, leggings or tight jeans should be avoided, including Lycra. Wear loose-fitting trousers or skirts and replace tights with stockings. At home, patients may find it more comfortable to wear long skirts without underwear.
• Sleep without underwear.
• Avoid fabric conditioners and biological washing powders. Consider washing underwear separately in a non-biological washing powder/gel.
• Some over-the-counter creams including baby or nappy creams, herbal creams (e.g. tea tree oil, aloe vera) and ‘thrush’ treatments may include possible irritants. Stop using them if they seem to be making things worse.
• Avoid antiseptic (as a cream or added to bath water) in the vulval area.
EMOLLIENTS (for all conditions)
Emollients can be used as moisturisers throughout the day. Please be aware that creams contain more additives than ointments so opt to prescribe OINTMENTS. If symptoms get worse or do not improve, stop using.
Formulary | Lothian Joint Formulary (nhs.scot)
• Using one of these moisturisers every day can help relieve symptoms. Even when asymptomatic, using a moisturiser helps to protect skin and can prevent flare-ups.
• It is important to find the moisturiser that works for the patient.
• If the skin is irritated, the emollient can be kept in the fridge and dabbed on to cool and soothe the skin.
CLOBETASOL PROPRIONATE 0.05% OINTMENT (for diagnosed/suspected Lichen Sclerosus and Lichen Planus only)
The Clobetasol ointment should be used sparingly (this means a fingertip sized amount on large areas but on smaller isolated areas a garden-pea sized amount) to the inner vulva and/or area around the anus. This ointment should not be used on other areas in the groin unless specifically directed by a medical professional.
Apply the ointment:
Morning and night for 1 month
At night for 1 month
Alternate nights for 1 month
Then 1-2 times a week for maintenance.
A 30g tube should last at least 6 months. This amount is very safe and should not cause adverse effects on the treated skin or elsewhere in the body. If symptoms return whilst on a maintenance treatment, the Clobetasol ointment can be used for a few extra nights to treat the flare-up and then try to reduce back to once weekly. It is normal to notice stinging for a few minutes after applying the ointment. However, if stinging in the area lasts for more than 1-2 hours after application, the patient may have been sensitised to one of the ingredients. An alternative should be used. Please note, sensitisation is more likely with creams rather than ointments due to the additional additives in the former.
Follow Up
- GP review 4-6 wks after instigating initial therapy.
- Self directed monitoring using a handheld mirror approx. 3-4monthly – if any concerns to be reviewed by GP
- Annual GP check
Patients should be given a detailed explanation of their condition with particular emphasis on any long-term implications for the health.
Patient information leaflets / professional information can be found at the sites below:
www.bssvd.org (The British Society for the Study of Vulval Disease)
www.bad.org.uk (British Association of Dermatologists)
www.issvd.org (International Society for Study of Vulval diseases)
https://vulvalpainsociety.org (Vulval Pain Society)
NZ Dermnet https://dermnetnz.org (DermNet NZ – All about the skin | DermNet NZ)- excellent Consultant Dermatologist written site on all Dermatology conditions incl vulval diseases.













