Please note that although the bowel screening programme and the Colorectal service (for symptomatic patients) both use quantitative FIT (faecal immunochemical test), the test threshold for further investigation is different for the two patient populations. In the asymptomatic population, the threshold used by screening is >80 mHb/g but in symptomatic patients, the threshold for investigation is >10 mHb/g. Hence, a person may have had a ‘negative’ FIT from screening but have a test value that is >10mg/g. Therefore, a person presenting with colorectal symptoms should not be advised to request a bowel screening kit as there is a risk that abnormal results and therefore significant bowel pathology could be missed. If someone presents with concerning colorectal symptoms, please refer as advised in the pathway below.
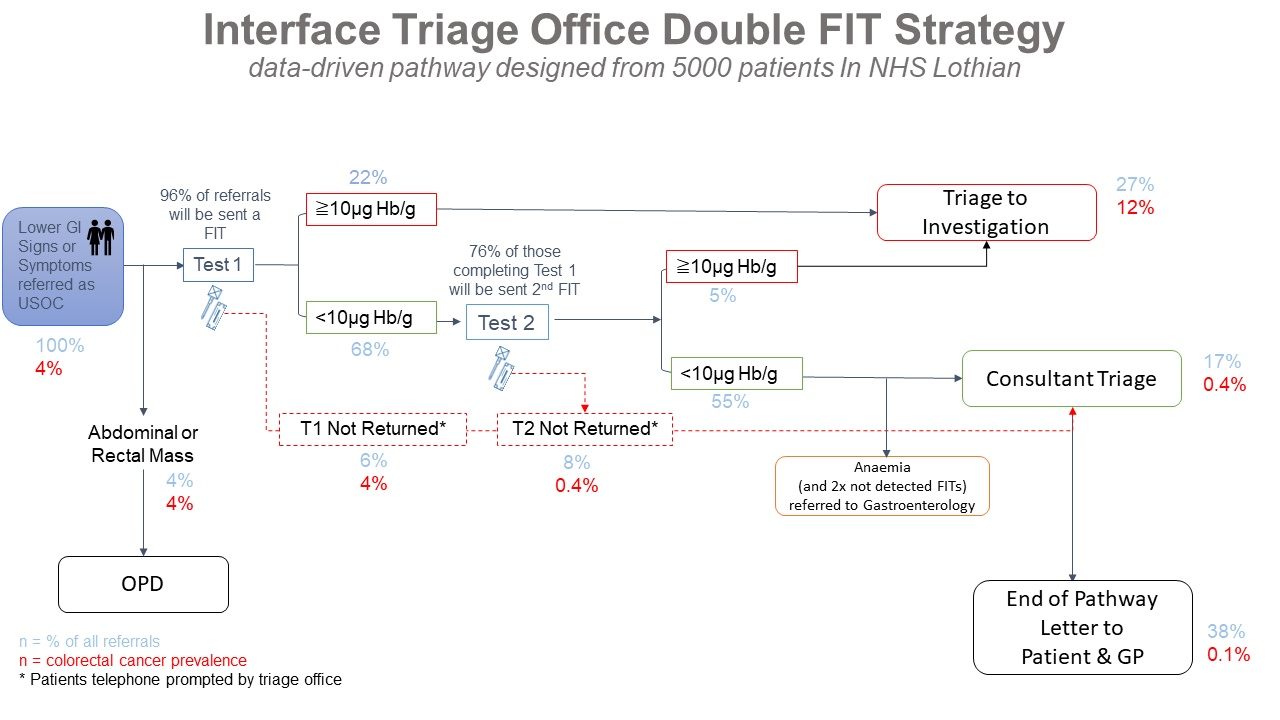
The Colorectal team have developed a diagnostic pathway, using multiple quantitative faecal immunochemical tests (qFITs), which aims to rationalise available resources and stratify patients according to likelihood of pathology. The triage pathway incorporates symptoms, qFIT results and patient frailty and co-morbidity to determine the next step which may be colonoscopy, CT colonoscopy or out-patient consultation.
qFIT requests will be generated from secondary care and the results will be interpreted, and appropriate clinical action taken, by secondary care. Patients will be asked to submit at least 2 qFIT tests.
The pathway seeks to get the patients with the greatest likelihood of pathology to the most appropriate test. Those with lower risk symptoms and normal qFITs may be offered a CT minimal preparation (plain CT with oral preparation) to safety net. Patients with 2 negative qFITs AND low-risk symptoms are unlikely to undergo further tests. There are some limitations with the new pathway and these measures may not detect all cancers and other diseases at an early stage. It has been devised to find gross abnormalities that need urgent intervention.
The final outcome of a set of tests will be communicated directly to patients by the triaging consultants, copied to the GP. Patients who have not completed the full set of investigations will be booked into a virtual clinic for the triaging consultant to assess the residual risk.
Who to refer:
Any patient with high risk features as detailed below:
| Bleeding | – Repeated rectal bleeding without an obvious anal cause – Any blood mixed with the stool |
| Bowel habit | – Persistent (more than four weeks) change in bowel habit especially to looser stools – not simple constipation) |
| Mass | – Unexplained abdominal mass – Palpable ano-rectal mass |
| Pain | – Abdominal pain with weight loss (also consider upper GI cancer) |
| Iron deficiency anaemia | – Unexplained iron deficiency anaemia See detailed advice regarding this at: https://apps.nhslothian.scot/refhelp/Gastrointestinal/IronDeficiencyAnaemia and refer via Sci Gateway “iron deficiency anaemia” pathway under Gastroenterology if this is the only symptom |
If symptoms suggestive of malignancy i.e. weight loss or other non-specific symptoms (without iron deficiency anaemia) in the absence of GI symptoms consider direct referral for CT via GP access pathway: https://apps.nhslothian.scot/refhelp/guidelines/GPAccesstoCTforSuspectedCancer(NoClinicallyObviousPrimary).aspx
Consider the possibility of ovarian cancer in any woman over 50 years who has experienced new symptoms within the last 12 months that suggest irritable bowel syndrome.
How to refer:
Via Sci Gateway to Colorectal Surgeons at the WGH or SJH via the “Urgent Suspicion of Cancer” pathway.
Please indicate if a patient is frail +/- has co-morbidities because this may influence if, and what, further investigations are appropriate. Please also establish that the patient wishes to be investigated and is willing to attend the hospital for appointments.
All patients should have the following before referral:
- Abdominal examination
- PR examination
- FBC, U&Es, LFTs (within the last 6 weeks)
These may also be appropriate for some patients:
- If constipation: TFTs, Calcium
- If diarrhoea: Faecal calprotectin (those under 40 years old) and stool culture
- Coeliac screen (anti tTG antibody)
- CA125 and pelvic US scan
A 4-week Watch & Wait Policy is reasonable in those with Low-risk features such as:
- Transient symptoms (less than 4 weeks)
- Patients under 40 years in absence of high-risk features
Watch and wait Policy (4 weeks)
- Assessment and review
- Consider bowel diary
- Appropriate information, counselling and agreed plan for review with GP
- Refer if symptoms persist or recur













