Key messages
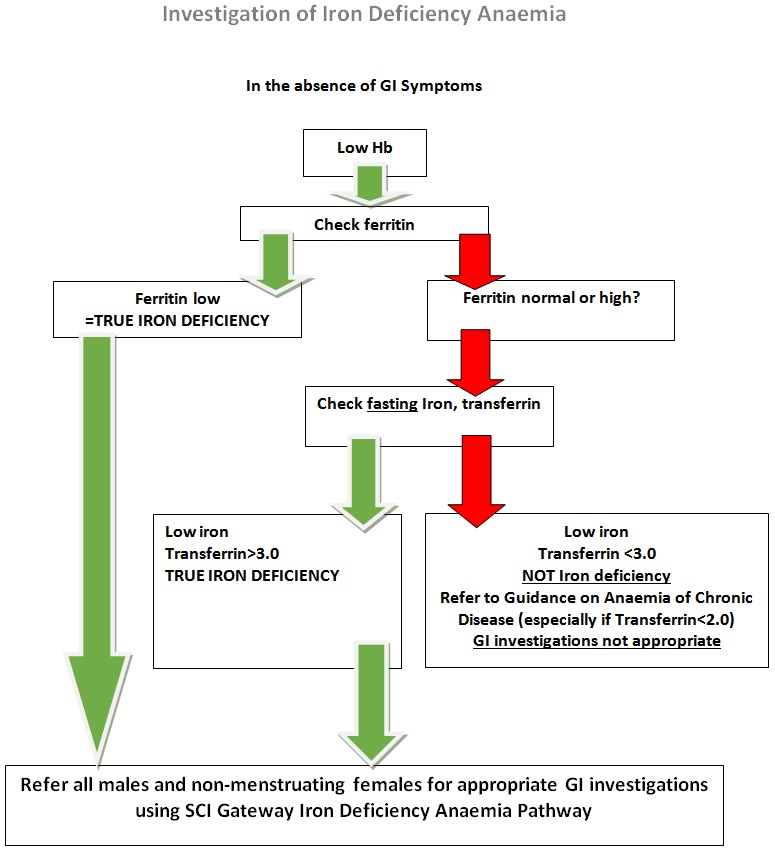
- Iron deficiency anaemia is defined as a low haemoglobin in the presence of either
- Low ferritin (best diagnostic marker)
- Low serum iron in the presence of transferrin >3.0
- The prevalence of iron deficiency anaemia amongst adult males and non-menstruating females in the developed world is approximately 2-5%
- Iron deficiency anaemia can arise as a consequence of
- Loss of iron (menstrual blood loss, GI blood loss, renal tract blood loss)
- Malabsorption (previous gastric surgery, Coeliac disease)
- Poor dietary iron intake (poor diet, lifestyle choices or cultural beliefs)
- May be contributing factors:
- Menstrual blood loss is the commonest cause overall
- Testing for Coeliac disease (anti tTG antibodies) is worthwhile
NOTE THAT IRON AND TRANSFERRIN SHOULD BE DONE ON A FASTING SAMPLE
In the presence of true, proven iron deficiency, approximately 10% of males and non- menstruating females will have a significant GI problem underlying this.
- These individuals should be referred for appropriate GI investigations if they are sufficiently fit to undergo them
- Investigation of the upper and lower GI tract will be undertaken
- Upper GI Endoscopy combined with either
- Colonoscopy or CT colonography or minimal preparation CT scan
- Appropriate investigation will be at the discretion of the secondary care team and will depend on a patient’s age and general fitness (which may have to be determined by clinic visit first)
- CT colonography will be offered to less fit patients or those who cannot tolerate colonoscopy*
- Minimal prep CT (no purgative laxative preparation) will be reserved for the most frail patients where any investigation at all is appropriate*
- *It would be useful to have up to date U&E’s for frail patients or those >80 years
GI investigations are not appropriate in other types of anaemia unless there are clear GI symptoms to be investigated
- Menstruating females should not undergo GI investigation in the absence of GI symptoms or a family history of colon cancer
- Testing for Coeliac disease is appropriate in these patients
- GI investigations may be appropriate for patients >50 years (and without history of menorrhagia) with proven iron deficiency in the absence of anaemia
Males and non-menstruating females who have Iron Deficiency Anaemia, in the absence of GI symptoms, should be referred using the Iron deficiency Anaemia pathway via Gastroenterology.