Background
PCOS is very common, with prevalence in women of reproductive age of 5-10% – and some estimate much higher. It is probably more common in women of South Asian origin. Many women with the condition are overweight or obese.
Women with PCOS have an increased risk of insulin resistance which, with the high prevalence of obesity, is a powerful risk factor for progression to Type 2 diabetes: note that insulin resistance is raised even in women with PCOS and a normal BMI.
There is also an increased long-term risk of endometrial hyperplasia/cancer, but no apparent increased risk of breast or ovarian cancer. Currently, despite having a number of risk factors for cardiovascular disease, it is unclear whether the actual risk is increased.
Diagnosis of PCOS
A diagnosis of PCOS requires at least 2 of the following 3 criteria: –
- Infrequent menses (>35 days between menses) or amenorrhoea >3 years post menarche
- Clinical and / or biochemical signs of excessive androgen secretion, i.e. hirsutism, acne, raised total testosterone or a raised Free Androgen Index (FAI). Although raised LH, with a normal FSH, may be found in PCOS, gonadotrophin results no longer form part of the diagnostic criteria.
- Presence of at least 12 follicles measuring 2-9 mm in diameter, an ovarian volume > 10ml3, or both by ultrasound (preferably transvaginal). This criterion does not apply to adolescents, for whom ultrasound is less helpful.
Lothian guidance is that a scan for suspected PCOS is not required unless there are other indications e.g. pelvic symptoms: THE DIAGNOSIS IS PRIMARILY MADE ON CLINICAL AND BIOCHEMICAL FEATURES.
Other possible causes of presenting features should be considered and excluded:
- congenital adrenal hyperplasia (CAH)
- androgen secreting tumour
- Cushing’s syndrome
- thyroid dysfunction
- hyperprolactinaemia and perimenopause etc.
These generally are excluded with basic blood tests and clinical features. The most important pointer to the possibility of CAH, androgen secreting tumour or Cushing’s syndrome is Testosterone >4nmol/l* or clinical features such as rapidly-developing hirsutism.
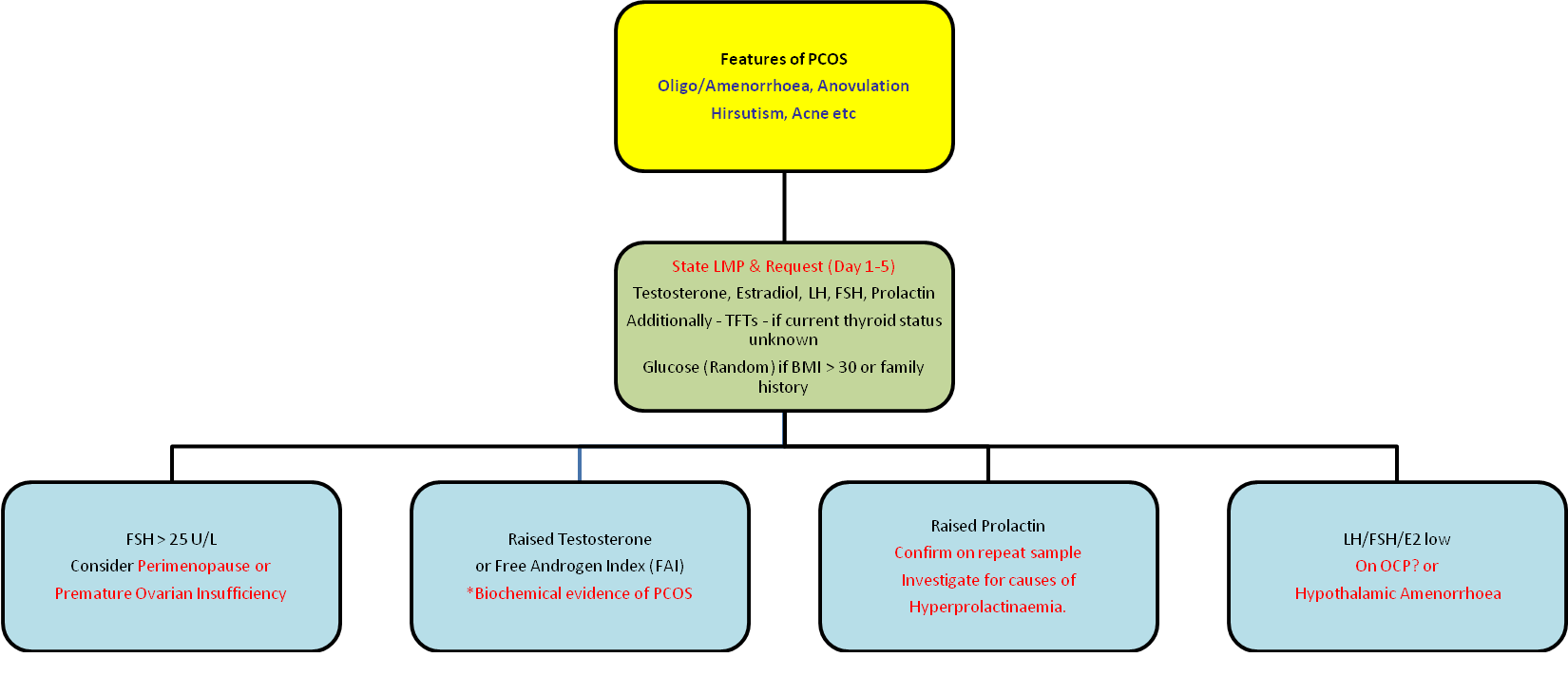
Laboratory investigation of patients with suspected PCOS
Sample Timing
Unless the patient is amenorrhoeic, the sample should be taken on days 1-5 of the menstrual cycle (misleading increases in testosterone may occur later in the cycle).
Clinical details
- State the LMP
- If there is amenorrhoea, state this on the request form.
- Provide clinical details e.g. hirsutism, irregular periods etc.: these are crucial as the laboratory may add additional tests.
Test requests
- LH, FSH, Estradiol, Testosterone & Prolactin as first line
- TFTs if thyroid status unknown
- random glucose (if BMI is > 30 kg/m2 or family history of diabetes), and HbA1c if glucose is borderline as per Lothian guidelines.
The laboratory will add any necessary additional tests (e.g. free androgen index (FAI), dehydroepiandrosterone sulphate (DHEAS), 17 hydroxyprogesterone, androstenedione) in the light of the results and the clinical details provided. To facilitate this it is crucial to provide all relevant clinical details.
Reports
An Endocrine Biochemist will issue an interpretative comment on all results – if adequate clinical details have been provided – and indicate what additional action regarding further sampling etc. is advised. The Endocrine Duty Biochemist can be contacted on 0131 242 6880
* It is unusual for PCOS to present with a testosterone of >4 nmol/L: in such patients the test should be repeated as soon as possible. If confirmed on repeat sampling, the patient should be referred for an endocrine opinion.
Additional notes for interpretation of blood results in PCOS
LH
- Increases in LH & LH/FSH ratio occur in many women with PCOS
- However LH is often normal in PCOS and is not required for the diagnosis
- Measurement of LH (and FSH and estradiol) can be useful in identifying other causes of amenorrhoea eg the low gonadotrophins & estradiol of ‘functional’ or ‘hypothalamic’ amenorrhoea associated with weight loss, stress and excess exercise. In these conditions, LH is generally more suppressed than FSH, and FSH concentrations can be normal.
Prolactin
- Up to 40% of women with PCOS have mildly elevated prolactin concentrations – generally <750 mIU/l (relating to unopposed estrogen).
- In PCOS the LH will be higher than the FSH – unlike true hyperprolactinaemia where the LH concentrations are lower than the FSH concentrations (and estradiol concentration may also be low).
- Prolactin can be increased due to pituitary adenomas
- Multiple other causes for increased prolactin – including stress, drug treatment (dopamine antagonists), hypothyroidism and unopposed estrogen.
- See Endocrine guidance for investigation of hyperprolactinaemia Endocrinology if Prolactin >1000mIU/l
Testosterone and free androgen index (FAI)
- Testosterone production roughly doubles in the early follicular phase when it may rise above the upper reference limit. Therefore if a patient is having periods, a sample taken during/shortly after menses (day 1-5 of cycle) is the most suitable for PCOS diagnosis to avoid a misleadingly-high testosterone result later in the cycle
- A large proportion of circulating testosterone is bound to sex hormone binding globulin (SHBG).
- SHBG-bound testosterone is biologically inactive cf its unbound or ‘free’ form
- Serum SHBG is decreased (and therefore active testosterone increased) in: PCOS, insulin resistance, obesity, hyperprolactinaemia, hypothyroidism and when there are high serum androgens.
- Serum SHBG is increased (and active testosterone reduced) by: estrogen, pregnancy, hyperthyroidism, excess alcohol, liver disease and anticonvulsants.
The free androgen index (FAI) is a simple method of estimating the circulating free testosterone in women but may be unreliable in situations where there are extreme abnormalities in the concentration of SHBG.
- The FAI is more sensitive at detecting hyperandrogenism than total testosterone, and may be helpful in assessing androgen status where total testosterone is in the upper half of the reference range.
- If total testosterone is in the lower part of the reference range, FAI is generally not raised.
- As PCOS is associated with reduced SHBG levels, this increases the FAI (i.e. active, free hormone), while total testosterone can remain normal.
See Gynaecological Radiology & Poly Cystic Ovary Syndrome
Who to refer:
- Diagnostic uncertainty
- More specialist management – e.g. when first line therapy is ineffective or contraindicated.
- When infertility in the primary issue ( see infertility EFREC guidance ). Referral does not require a duration of trying for a pregnancy.
- When a repeat testosterone remains over 4nmol/L, please refer to endocrinology.
Most women with PCOS are successfully managed symptomatically in primary care. However, when there are specific concerns about the diagnosis or questions around information provision or more specialised management strategies, (such as for hirsutism or where the COCP is not suitable) in the short or long term.
Who not to refer:
When weight is the primary issue.
How to refer:
The most appropriate place for referral is the specialised Reproductive Endocrine clinics based in EFREC at the Royal Infirmary of Edinburgh. Women with PCOS and anovulation seeking help with fertility should be referred immediately without the one-year requirement.
Referral to General Endocrinology may be more appropriate if the patient has existing diabetes or co-morbid endocrine problems.
1. Diagnosis and explanation to patient
2. First line Rx – supportive and lifestyle including diet /exercise etc and management of obesity etc (we can link to the weight management section here Weight Management Service Adult).
3. Management of oligo/amenorrhoea:
- It is recommended that menses occur at least every 3 months to provide endometrial protection against hyperplasia and potentially cancer.
- If contraception is not required, endometrial protection can be readily achieved by periodic progestogen therapy e.g. medroxyprogesterone acetate 10mg bd for one week or 10mg od for 10-14 days. This allows the patient to be in control of precise timing.
- COCP will often be the most effective treatment, also providing contraception.
- Mirena IUS will also provide effective protection.
- Any gestagen containing contraception such as the POP or subdermal implant will provide endometrial protection
4. Management of metabolic risks
- Women with PCOS are at increased risk of impaired glucose tolerance and T2DM: please see ECED on www.edinburghdiabetes.com for more detail. Weight reduction and lifestyle modification is important as is screening for diabetes in obese women with PCOS.
- Consider sleep apnoea in women with PCOS
5. Management of hirsutism and acne
ACNE – please refer to dermatology guidance for standard management.
HIRSUTISM is very subjective and while there are scoring systems for research use, they are of little value in clinical practice. For those needing treatment:
- Hirsutism: first line therapy is cyproterone acetate (CPA) formulated as per COCP (co-cyprindiol 2000/35) unless contraindicated. However other COCPs have similar efficacy. This may take 6 months to show an effect, but that effect increases over at least 2 years.
- Eflornithine cream may also be useful. It can irritate the skin, but may act more quickly that CPA.
6. Psychological and psychosexual issues.
- Women with PCOS often suffer from low self-esteem, thus psychological support can be required.













