History
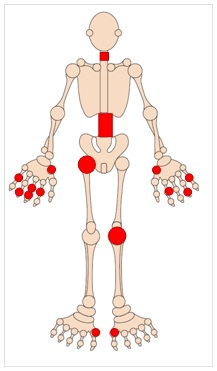
- Pain and affecting PIP, DIP and 1st CMC joints.
- Knee pain (worse on descending stairs)
- Hip pain worse on weight bearing
- Back, neck and shoulder girdle pain
- Age at onset usually >50.
Examination
- Bony swelling of affected joints in the hands
- Crepitus on knee flexion
- Limitation of hip movement
- Pain on back, shoulder and neck movement
Investigations
- Routine bloods (usually normal)
- Anti-CCP antibodies (negative)
- X-ray of symptomatic joints (loss of joint space andosteophytes)
M.A & H.B/S.R 25-01-24
Patients with osteoarthritis should not be referred to Rheumatology unless there is uncertainty about the diagnosis.
No therapies are available to slow or halt the progression of osteoarthritis.
Treatment is symptomatic.
Patient Education:
- Making patients aware that this is wear and tear of the joints and that although there is no cure, several treatments can help symptoms.
Non-pharmacologic:
- Weight loss can make a big difference in patients with hip or knee OA.
- Exercise will improve symptoms
Nutraceuticals:
- Glucosamine and chondroitin may have a weak effect on pain (not recommended by NICE)
Manual therapy:
- Only consider for hip and knee osteoarthritis and alongside therapeutic exercise.
Pain Management :
Start with local therapy and add additional medications as necessary. It’s possible to use analgesics, NSAID and anti-neuropathic drugs in combination.
- Topical NSAID cream
- Paracetamol
- Oral NSAID (with PPI)
- Compound analgesics
- Anti-neuropathic agents (gabapentin or amitriptyline)
- Strong opioids as last resort
Orthopaedic referral: Consider in patients with x-ray confirmed hip or knee OA showing significant loss of joint space in whom there has been an inadequate response to medical treatment
Please see Resources and links tab for additional information
- Osteoarthritis (OA) | Causes, symptoms, treatments (versusarthritis.org)
- 2022 NICE guideline for the diagnosis and management of osteoarthritis (nice.org.uk/guidance/ng226)













