Hypertension in the postnatal period
Information
Hypertensive disorders during pregnancy affect around 8-10% of all pregnant women and can be associated with substantial complications for the woman and the baby including maternal morbidity, stillbirths, neonatal deaths and perinatal morbidity. Women with hypertension in pregnancy are also at increased risk of CVS disease in later life. Up to 40% of hypertensive disorders of pregnancy can emerge in the early postnatal period.
Who can refer:
- GP
- Community midwife
Who to refer:
Consider the possibility of pre-eclampsia or eclampsia in the postnatal period if a woman develops any of the following:
- Severe headaches, increasing frequency, unrelieved by analgesia
- Visual problems
- Persistent new epigastric or RUQ pain
- Vomiting
- Hypertension >140/90
- Proteinuria
- Sudden onset SOB due to pulmonary oedema
- Sudden swelling of hands, face or feet
- Seizure within 4 weeks of birth
If concerns about pre-eclampsia or very high BP (160/110mHg) – urgent referral to Obstetric Triage Assessment at Royal Infirmary (0131 242 2657) or labour ward at St John’s Hospital (01506 524125), or contact the Obstetric Registrar On Call via Switchboard at Royal Infirmary / St John’s Hospital.
How to refer:
For emergencies and urgent care, patients can come without calling.
However, if possible, the patient should phone for advice first. There is a midwife who is available 24/7:
Royal Infirmary of Edinburgh 0131 242 2657
St John’s Hospital 01506 524125
For women with existing hypertension
Suggested monitoring
- Daily for the first 2 days after birth, once between days 3-4, then as clinically indicated
thereafter, usually every other day for 2 weeks. This can be completed by the community midwives.
Suggested treatment
- Continue antihypertensives
- Methyldopa should have been stopped after birth
- Restart antihypertensive treatment from before pregnancy unless breast feeding
- Medical review at 6-8 weeks
For women with gestational hypertension
Suggested monitoring
- Daily for the first 2 days after birth, once between days 3-4, then as clinically indicated
thereafter. This can be completed by the community midwives.
Suggested treatment
- For women discharged on antihypertensives – continue medications, monitor BP as above and reduce doses as required
- Duration will usually be similar to duration of antenatal treatment but may be longer
- Medical review 2 weeks after transfer to community care and at 6-8 weeks
- Target BP is 140/90
- If gestational hypertension not on treatment, consider initiation of treatment if BP >140/90, Review at 6 weeks if gestational hypertension not on treatment
Postnatal hypertension
Blood pressure peaks days 3-6 postnatal and BP should be checked postnatally to identify late pre-eclampsia. This can be completed by the community midwives.
Suggested monitoring
- Daily for the first 2 days after birth, once between days 3-4, then as clinically indicated thereafter.
Suggested treatment
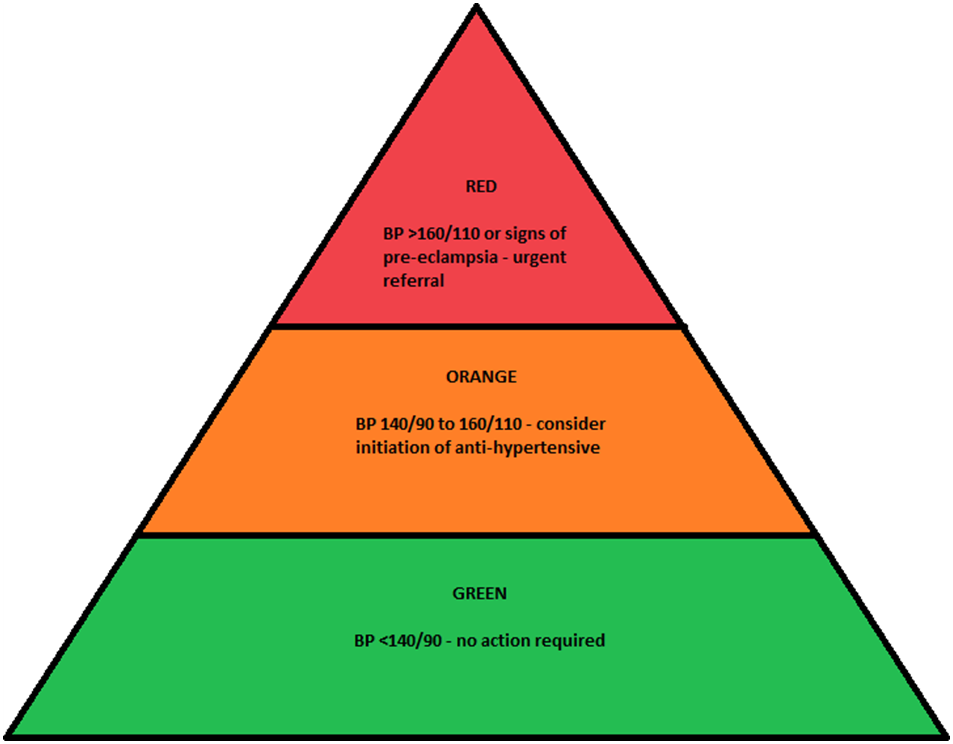
- Aim <140/90. If BP >140/90 – consider commencing antihypertensive – see table below if breastfeeding
- If not breastfeeding postnatally – manage as per NICE guideline for hypertension in adults.
- If BP >160/110 or symptomatic – refer to Obs Triage for urgent assessment
Ongoing Follow Up
- All patients should have a repeat urine dipstick for protein at 6 weeks, if not resolved please send urine PCR and for further review at 3 months. If ongoing proteinuria or abnormal renal function consider referral to renal physician as appropriate
- If hypertensive and <40 – for investigation for secondary cause as per guidelines
- If hypertensive and >40 – for management as new adult essential hypertension
- Women with pregnancy induced hypertension in the long term have high rates of chronic hypertension, cardiovascular disease and thromboembolism.
- Consider using ASSIGN or QRISK in women over 30 who have had hypertension during pregnancy, even if resolved following delivery.
- Life style changes – Smoking cessation, weight management, low salt diet and regular exercise encouraged.
Antenatal Hypertension medication recommendations used in NHS Lothian
| Drug | Place in Therapy | Starting dose | Max Dose | Contraindication | Breastfeeding |
| Labetalol | 1st line | 100mg BD | 600mg QDS | Asthma | Yes – only small amounts in breast milk |
| Nifedipine (Coracten SR) | 2nd line | 10mg MR BD | 40mg MR BD | Yes – amount too small to be harmful, manufacturer suggests avoid but widely used without reports neonatal effect | |
| Methyldopa | 2nd line | 250mg BD | 1g TDS | Depression | Yes |
| Hydralazine | 2nd line | 25mg TDS | 75mg QDS | Yes |
Postnatal hypertension medication recommendation if breastfeeding – if not breastfeeding as per Adult Hypertension guidelines
| Drug | Place in Therapy | Starting dose | Max Dose | Contraindication | Breastfeeding |
| Enalapril | 1st line – requires K and renal function monitoring | 5mg OD | 40mg OD | Yes – low concentrations excreted, probably too small to be harmful | |
| Nifedipine (Coracten SR) | 2nd line | 10mg MR BD | 40mg MR BD | Yes – amount too small to be harmful, manufacturer suggests avoid but widely used without reports neonatal effect | |
| Labetalol | 3rd line | 100mg BD | 600mg QDS | Asthma | Yes – only small amounts in breast milk |
NICE guideline 133: Hypertension in Pregnancy- Diagnosis and Management – 25th June 2019
Overview | Hypertension in pregnancy: diagnosis and management | Guidance | NICE













