Headache ‘Plus’ (CT Head for Urgent Suspicion of Cancer) Pathway
Please note – There are 2 Open Access CT Head Pathways on SCI Gateway.
- WGH > Neuroradiology > LI Neuroradiology
OR
2. WGH> Neuroradiology > Headache suspect brain cancer
This pathway is for patients with a headache and there is a suspicion of brain cancer/tumour. It is not for routine CT for patients with Chronic Headache alone. (For guidance for these patients please see the Neuroradiology and Headache pages.)
Headache alone as a presenting symptom of brain cancer is rare. There is less than 0.5% chance of a relevant finding and a 1:10 chance of an incidental finding, that may cause anxiety. The radiation dose of a CT head is 100 chest x-rays. Studies suggest it does not provide long lasting reassurance.
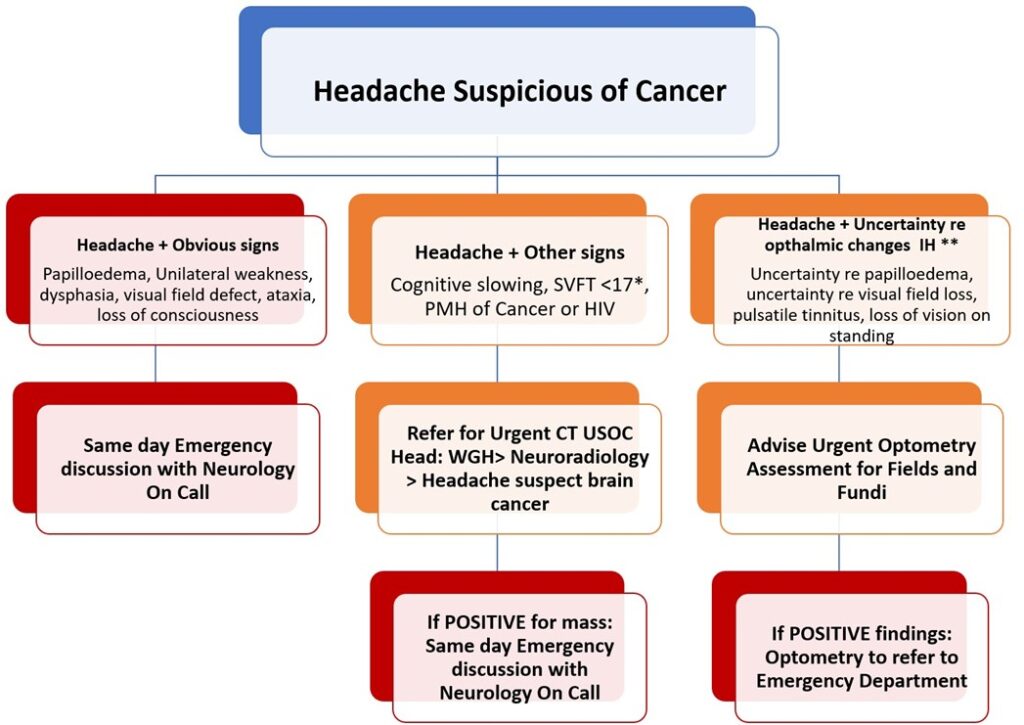
The aim of this pathway is to stratify the urgency of CT Head and improve diagnostic yield of CT Heads for Brain Cancers.
A Headache, ‘Plus’ the addition of cognitive and other symptoms increases the positive predictive value of the CT Head.
* SVFT = Semantic Verbal Fluency Test
** IH = Intracranial Hypertension
Who to refer:
Headache (of concern, where other headache diagnoses are considered less likely)
“Plus” any of the following:
a) Cognitive slowing: memory, concentration or personality change
b) Semantic verbal fluency score (SVFT) (“How many animals can you think of in a minute?”) < 17 animals +/- cognitive complaints is significant.
c) A PMH of Cancer or HIV
———
d) Headache + Focal symptoms (Papilloedema, unilateral weakness, dysphasia, visual field defect, ataxia)
e) Headache + Loss of Consciousness
———
f) Uncertainty re disc Papilloedema or Visual field loss
g) Headache + Pulsatile tinnitus or Visual obscuration on standing (loss of vision)
Outcomes:
- Headache plus a, b or c: Urgent Open Access CT scan (USOC – Urgent Suspicion of Cancer) (Done within a few days).
- Headache plus d or e: Urgent discussion with Neurology on call.
- Headache plus f or g: Urgent referral to optometry for check of discs and fields within 24-48 hours. If Papilloedema ultimately found to be present – Optometrist/GP to Refer to urgently (same day) to neurology.
Other considerations:
- Sudden onset – Suspected Subarachnoid Haemorrhage – Same day referral to neurology.
- Over 65 and new headache with no significant headache history – Either discuss with neurology or refer CT Head – USOC
- Progressive – Postural/Valsalva induced headache – Either discuss with neurology or refer CT Head – USOC
- Pregnancy – Check RefHelp Neurology> Headaches and discuss with a neurologist if needed.
- Phenotype (of a rare headache) – Check RefHelp Neurology> Headaches and discuss with a neurologist if needed.
How to refer:
Using SCI Gateway:
- WGH> Neuroradiology > Headache suspect brain cancer
(Please note that DCN is now based at the RIE, however the referrals should still be sent to the WGH. When this changes this webpage will be updated and all GPs will be informed by email.)
Who not to refer:
Do not use this pathway if:
- Low risk features/headache only – Patients with symptom of a headache alone, and in whom CT Head has a low positive predictive value. After discussion with the patient about the potential consequences and outcomes of CT Head, they can be referred for non-urgent CT Head using the alternative SCI Gateway pathway: WGH > Neuroradiology > LI Neuroradiology.
- Headache with definite Papilloedema – Requires emergency (same day) referral to neurology
For information on headaches where brain tumour is not likely to be the cause see https://apps.nhslothian.scot/refhelp/Neurology/Headache
Background to the Pathway
The Edinburgh direct access CT head route for headache has been available for >10 years. This is not based on any specific protocol. Cases with headache were audited. (Zienius, K., Chak-Lam, I., Park, J. et al. Direct access CT for suspicion of brain tumour: an analysis of referral pathways in a population-based patient group. BMC Fam Pract 20, 118 (2019). https://doi.org/10.1186/s12875-019-1003-y) https://bmcfampract.biomedcentral.com/track/pdf/10.1186/s12875-019-1003-y.pdf
- Over a 5-year period, 3257 head scans were performed (318 scans excluded).
- 53 patients (1.8%) were reported to have intracranial tumours
- 42 were significant (diagnostic yield of 1.43%)
- 11 were incidental.
- There were no false negative CT scans for tumour.
- 559 patients had non-tumour findings,
- 31% of which were deemed clinically significant.
- In 34% of the 559 patients (190) – referral for further imaging and/or specialist assessment from primary care was still thought warranted.
Waiting times for scans was about 3-4 weeks
Headache alone as a presenting symptom of cancer is rare. New headache alone PPV for brain tumour = 0.1.
Headache “plus” the addition of cognitive symptom increases the PPV to 5.9
https://bmjopen.bmj.com/content/bmjopen/9/8/e029686.full.pdf
In 2017, a Edinburgh Protocol Based Referral Protocol was produced for cases with Headache (Suspicious of Cancer) “Plus” to stream more urgent cases for faster CT scans. Selection was based on GP opinion, but certain red flags were required to assess the value of these and a semantic verbal fluency score (how many words can you think of in a minute). These scans were done within a week. The SVFT did not affect the speed of the scan but all cases where a SVFT was performed had faster scans – as they were protocol complete – versus those referred through this pathway where SVFT was not complete.
The SVFT is a fast screen for cognition and has been used as a screen in dementia (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5619418/). A score <17 indicates concern for cognition (https://www.verywellhealth.com/verbal-fluency-test-and-how-it-screens-for-dementia-98629). The Sematic verbal fluency score has also been used as a screen for incipient cognitive problems in Parkinson’s Disease (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3655231/ ), Multiple Sclerosis for attention, executive dysfunction and memory (https://www.frontiersin.org/articles/10.3389/fneur.2020.629183/full) and also for brain tumour (https://www.researchsquare.com/article/rs-217313/v1 ), where it showed a moderate to strong correlation between MMSE and ACE-R, but was more sensitive and scores <10 words in a minute correlate with lack of capacity to consent (https://pubmed.ncbi.nlm.nih.gov/24991034/ and (https://link.springer.com/article/10.1007/s11912-019-0793-3).
The Edinburgh protocol was audited after year 1 (https://abstracts.ncri.org.uk/abstract/headache-suspicious-of-cancer-the-edinburgh-early-diagnosis-pathway/ ) and after 3 years (https://www.bnosconference.co.uk/wp-content/themes/wordpress-template/pdf/bnos_2021_abstract_book.pdf p34-35). The findings have been presented at the British Neuro-Oncology Society Meeting (July 2021) and the National Cancer Research Institute Annual Meeting (Nov 2021). To summarise:
- From March 2017-Nov 2019 there were 669 PBR for Headache SoC (62% female; Mean age 53 years).
- Ave time to scan <7 days
- SVFT were completed in 381 (57%). Median SVFT was 17 animals/minute.
- 11 cases (2.9%) had cancer. 10 of the 11 (91%) SVFT <17 (median 10 animals)
- SVFT was <17 in 188 HA SoC cases overall – 5.32% had a tumour
- Other causes for a low SVFT <17 were: 12 not native English speaker; 6 PMH brain injury; 19 co-existing dementia/MCI; 5 small vessel disease; 4 cysts (pineal / arachnoid); 4 Giant Cell Arteritis; 2 Chiari 1 malformations.
- 53 with SVFT <17 had current or PMH Psychiatric or Pain Clinic conditions and were taking (opioid analgesics/ antidepressant /antipsychotics). None had a brain tumour.













