There is helpful, patient-friendly information and advice to be found on the GI section of the NHS Lothian Internet pages. There are also some videos by our very own GI team which patients have been responding very positively to. Consider sharing the link with patients and/or carers.
https://services.nhslothian.scot/GI/IBS
How Doctors Make a Diagnosis of IBS
IBS Introduction
Background:
- Irritable bowel syndrome (IBS) affects 10-20% of the adult population
- Females are twice as likely to present as males
- Symptoms are most common in those ages 20-30
Consider a POSITIVE diagnosis of IBS in patients with any of the following symptoms for >6 months:
- Abdominal pain related to defaecation
- Change in bowel habit
- Change in stool form
features such as bloating, lethargy, nausea, backache and bladder symptoms are common in people with IBS and may be used to support the diagnosis
IBS Diagnostic Pathway
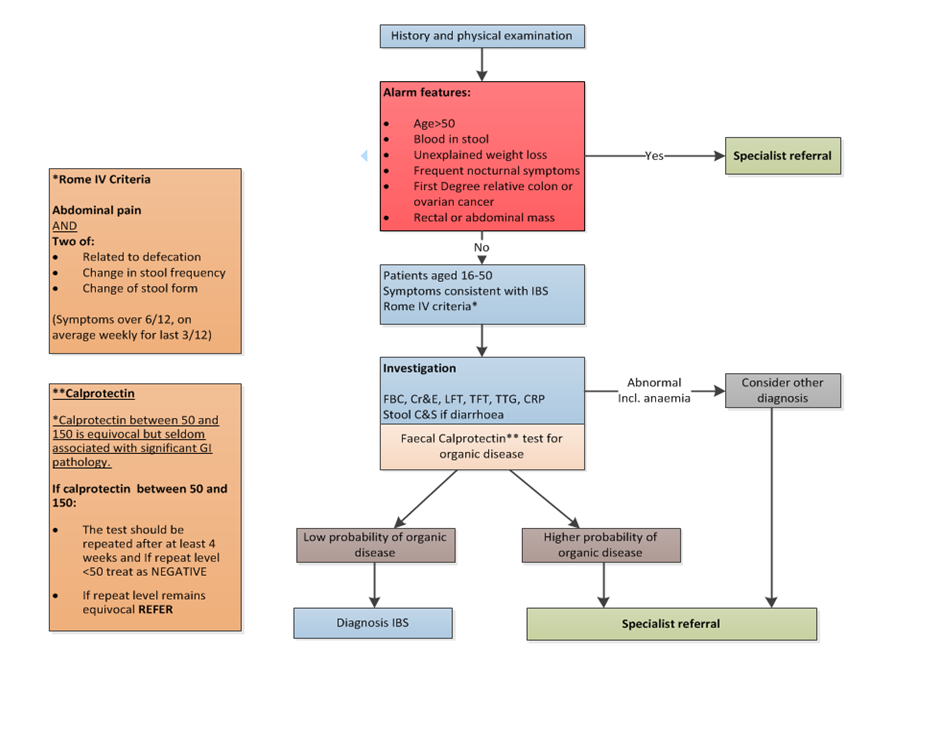
NOTES.
- Family history of colon cancer is especially relevant if a first degree relative (FDR) <50yrs is affected, or if there are 2 FDRs affected at an older age.
- Faecal calprotectin is useful in identifying patients with a higher probability of organic colonic disease. Availability, assays and protocols for the use of these tests vary, and local guidance on their usage and interpretation should be followed.
- In patients with persistent watery diarrhoea not responding to Rx, consider the possibility of microscopic colitis and possible need for colonic biopsies.
IBS Post-Diagnostic Management and Referral Pathway
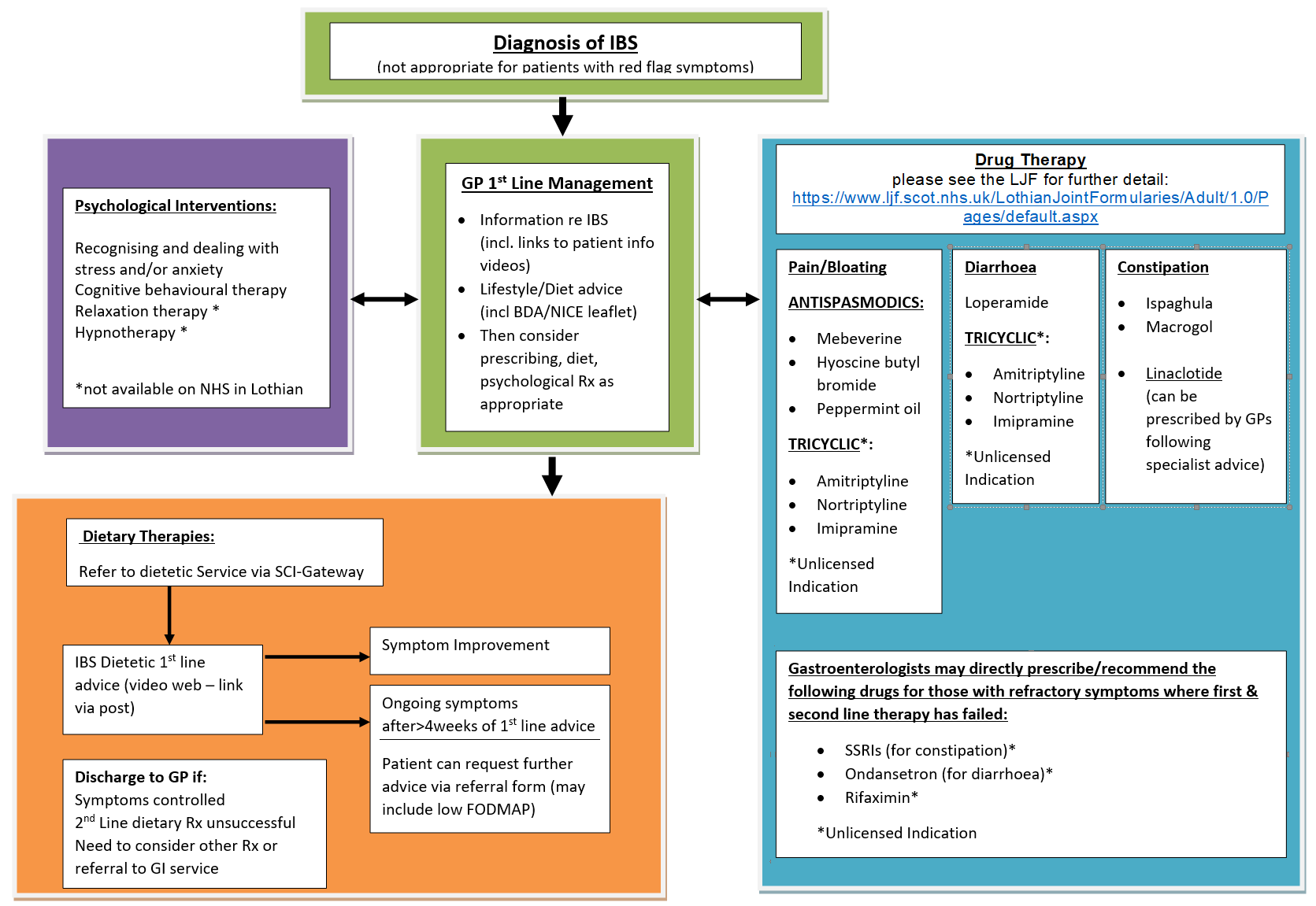
How to refer to the IBS (Post Diagnostic Pathway) on SCI: AHP – Dietetics – Adult IBS
General points
- Irritable Bowel Syndrome is NOT a diagnosis of exclusion
- It can be diagnosed POSITIVELY using simple clinical criteria and ruling out certain red flag symptoms and other conditions by simple tests available in Primary Care (see separate IBS Overview)
- Once a POSITIVE diagnosis has been made, treatment is consists of reassurance and symptom relief.
- This requires a very good understanding of what the symptoms are so a good history is vital
- Asking the patient to complete a symptom diary over 4 weeks is very helpful in clarifying the main symptoms
- Different approaches to treatment work better for different individuals and it is often necessary to trial a number of different approaches before settling on one which is most effective.
- A failure of one or two therapies is frustrating but common. It is not, in itself an indication that the primary diagnosis is wrong.
Outline of therapy.
- Selection of diet, drug or psychological interventions will be influenced by patient preference and local availability. Combination approaches may be appropriate for some patients.
- Drug therapies “below the line” should currently be regarded as primarily for specialist initiation.
Management
- COVID vaccination in IBD
- Nice BDA IBS advice leaflet
- GI – PIL Lifestyle and foods in IBS Feb 17
- National Institute for Health and Care Excellence (NICE)
- Scottish Intercollegiate Guidelines Network (SIGN)
- Irritable Bowel Syndrome (nice.org.uk)
- NICE BDA IBS advice leaflet.pdf
- IBD Helpline 0131 537 1272













