R.C 18-05-23
- Diagnostic uncertainty
- Not responding to Primary Care Management
- Moderate or Severe disease I.e. recurrent lesions separated by normal skin with sinus tract formation and scarring or multiple lesions coalescing into inflammatory plaques involving most of the affected region
Hidradenitis suppurativa (HS) – also known as acne inversa- is a disease of apocrine glands and can affect axillae, groins, perineum and inframammary areas. It is a neutrophilic inflammatory condition with hyperkeratotic follicular occlusion causing blockage and subsequent follicular rupture.
HS can vary in severity of presentation, from scattered inflammatory nodules and pustules through to abscesses, sinus formation and scarring.
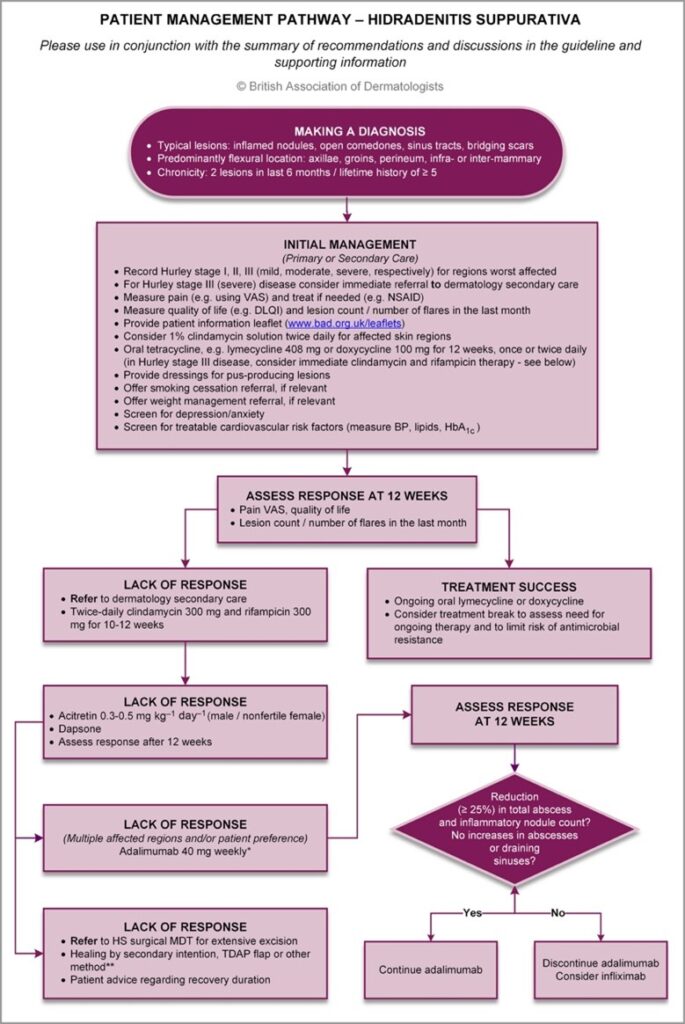
Diagnosis requires lesions to be chronic and recurrent and severity can be classified using scoring systems such as the Hurley Stages.
Consider HS where there are more than 2 abscesses in a flexural area in a six-month period. Early treatment is important to reduce progression to severe disease.
Factors associated with increased risk of HS include:
- Obesity
- Type 2 diabetes mellitus
- Smoking
- Polycystic ovary syndrome
- Family history (approximately 30% of cases)
- Female sex (post menarche/premenopause)
- Having Black or Mediterranean skin
HS can be associated with:
- Spondyloarthritis – including ankylosing spondylitis, psoriatic arthritis, rheumatoid arthritis, as well as generalised joint pains
- Acne
- Increased cardiovascular risk
- Crohn’s Disease (especially if groin/perianal lesions involved)
It can also form part of 2 uncommon familial syndromes:
- PASH syndrome: pyoderma gangrenosum, acne and hidradenitis suppurativa,
- PAPASH syndrome: Pyogenic arthritis, acne, pyoderma gangrenosum and hidradenitis suppurativa
General measures
- Advice and support re weight reduction
- Advice & support re smoking cessation
- Advice re unfragranced antiperspirants
- Advice re avoiding tight clothing or wearing synthetic materials
- Assess impact on mental health
- Screen for Type 2 diabetes & carry out CVD risk assessment
- Assess for associated spondyloarthritis/joint pains
Topical treatment
- 1% clindamycin solution applied twice daily to affected areas for 12 weeks. Avoid preparations with alcohol as this can irritate the skin.
- Antibacterial wash to reduce skin bacterial load (e.g. Dermol 500 or 4% chlorhexidine).
- Appropriate absorbent, non-adherent dressings to manage pus and reduce friction.
Systemic treatment
- Analgesia as lesions are usually painful.
- Lymecycline 408mg once daily or doxycycline 100mg once daily for 12 weeks.
- Consider starting clindamycin 300mg and rifampicin 300mg both twice daily for 10-12 weeks if severe disease. Remember that rifampicin prevents to COCP from working, so female patients of fertile age will need to use a robust alternative method of contraception. U&E and LFTs should be checked prior to starting. Maintain treatment if helps. Half doses of both medications may be appropriate if GI side effects are significant.
- Cyproterone acetate/ethinyl oestradiol COCP especially if cyclical flares.
- Consider metformin to reduce insulin resistance.
- Consider intralesional triamcinolone injection for large individual lesions.
Secondary Care treatments include:
- Acitretin or isotretinoin
- Dapsone
- Adalimumab
- Infliximab
- Surgical incision and drainage of individual lesions or excision of more extensive areas
For Patients
PIL Hidradenitis suppurativa https://www.bad.org.uk/shared/get-file.ashx?id=88&itemtype=document
There is an HS Support Group on Facebook but activity currently suspended. Can be accessed via PainUK website.
For Health Professionals
https://dermnetnz.org/topics/hidradenitis-suppurativa-severity-assessment
https://www.pcds.org.uk/clinical-guidance/hidradenitis-suppurativa