Supporting Information
Diagnostic Criteria
Diabetes and pre-diabetes may be diagnosed by any of the following criteria:
| Diabetes | Pre-Diabetes | Normal | |
| HbA1c (mmol/mol) | ≥ 48 | 42-47 | ≤ 41 |
| Fasting glucose (mmol/l) | ≥ 7.0 | 5.5-6.9 | ≤ 5.4 |
| 2-hr glucose in OGTT (mmol/l) | ≥ 11.1 | 7.8-11.0 | ≤ 7.7 |
| Random glucose (mmol/l) | ≥ 11.1 |
Types of Diabetes
Diabetes mellitus has many different causes. It is very important that the full potential differential diagnosis is considered in all new presentations of diabetes.
Type 1 Diabetes
This results from an absolute deficiency of insulin due to autoimmune pancreatic beta-cell destruction. It more commonly presents acutely in young people, but can occur at any age. A history of significant weight loss prior to diagnosis and the presence of ketones in the urine or blood are highly suggestive of type 1 diabetes. People with type 1 diabetes usually have detectable antibodies to GAD, IA-2 and/or ZnT8. Type 1 diabetes can occur in any individual regardless of age, ethnicity or weight. Therefore, measurement of blood or urine ketones should be performed in ALL individuals with a new diagnosis of diabetes.
Type 2 Diabetes
This results from a relative deficiency of and/or insensitivity to insulin and is more commonly diagnosed in older people, although can occur in young (especially obese) individuals. It is more common in people of South-Asian and Afro-Caribbean heritage.
Although the onset of type 2 diabetes is less dramatic than that of type 1 diabetes, the long-term sequelae are similar and equally devastating, as both Type 1 and Type 2 patients are at risk of developing the microvascular and macrovascular complications of the disease.
Monogenic Diabetes
These are rare forms of diabetes due to mutations in single genes; they are inherited in an autosomal dominant fashion. There are multiple different forms and the management principles depend on the specific gene involved. A diagnosis of monogenic diabetes should be suspect in individuals who do not demonstrate typical features of type 1 or type 2 diabetes. Further information about these forms of diabetes can be found at www.diabetesgenes.org
Pancreatic Diabetes (Type 3c diabetes)
Diabetes may be caused by disorders of the pancreas such as chronic pancreatitis, haemochromatosis, cystic fibrosis, pancreatic cancer and post-pancreatic surgery. The diagnosis of these forms of diabetes may be obvious depending on previous history, but these forms of diabetes should be considered in all individuals whose presenting features are not typical of type 1 or type 2 diabetes.
Steroid-Induced Diabetes
High doses of steroids, such as prednisolone or dexamethasone, can induce diabetes in susceptible individuals, i.e. older age and overweight. Individuals with an HbA1c in the pre-diabetic range (42-47 mmol/mol) are highly likely to develop diabetes if commenced on steroids. Consider checking an HbA1c in individuals at risk. If in the diabetes or pre-diabetes range then early commencement of blood glucose monitoring is recommended (see Steroid Safety guidance on RefHelp).
Pre-Diabetic States
Impaired Glucose Tolerance (IGT)
IGT is a state of impaired glucose regulation, diagnosed on glucose tolerance testing, which confers an increased risk of future diabetes of 2-5% per year. Patients with IGT tend to have higher blood pressure and plasma triglycerides when compared to non-diabetic individuals.
Impaired Fasting Glycaemia (IFG)
The term IFG classifies individuals with fasting plasma glucose (FPG) values above the normal range but below those diagnostic of diabetes i.e. FPG 6.1 mmol/L – 6.9mmol/L. All such individuals should have a HbA1c checked to exclude a diagnosis of diabetes (see diagnosis of diabetes in asymptomatic individuals)
Pre-diabetes
HbA1c between 42-47 is considered a pre-diabetic state.
Gestational Diabetes Mellitus (GDM)
GDM is defined as carbohydrate intolerance of variable severity with onset or first recognition during pregnancy. GDM is still diagnosed using an oral glucose tolerance test (OGTT) and this is essentially the only situation now when an OGTT should be performed in primary care. The diagnostic criteria are different to that for standard diabetes: fasting glucose ≥ 5.1 mmol/l and 2hr glucose ≥8.5 mmol/l. Women with risk factors for GDM, e.g. family history of type 2 diabetes, high risk ethnic group, previous large baby, elevated BMI, will have an OGTT arranged by their community midwife at 24-28 weeks.
Making a Diagnosis of Diabetes
Consider a diagnosis of diabetes in a person with potential symptoms of diabetes:
- thirst and polyuria
- unexplained weight loss or tiredness
- pruritus vulvae, balanitis or recurrent ‘UTIs’
- recurrent infections
- blurring of vision (usually an osmotic effect and not permanent)
Asymptomatic individuals at high risk of diabetes may also be screened:
- hypertension, cardiovascular disease
- obesity, especially if: BMI ≥30 kg/m2, high risk ethnic group, family history of Type 2 diabetes and/or learning disability
- long-term anti-psychotic medication, e.g. olanzapine, clozapine
- previous gestational diabetes (should have annual check of HbA1c)
- pre-diabetes (should have an annual check of HbA1c)
In individuals with a blood test diagnostic of diabetes, a repeat confirmatory test is required in those who are asymptomatic. The purpose of this is simply to ensure that there has not been a mis-labelling of a sample or a laboratory error. There is no minimum time limit as to when the repeat needs to be carried out (it can be done the same day!) and best practice is that it should be undertaken within 2 weeks. Best practice in people with a new diagnosis of pre-diabetes is that a repeat confirmatory test should also be carried out if the result is significantly different from a previous HbA1c result or out of keeping with the clinical picture. Guidance on the management of pre-diabetes is available on RefHelp; referral is recommended to the NHS Lothian Type 2 Diabetes Prevention Programme (via the Weight Management Service).
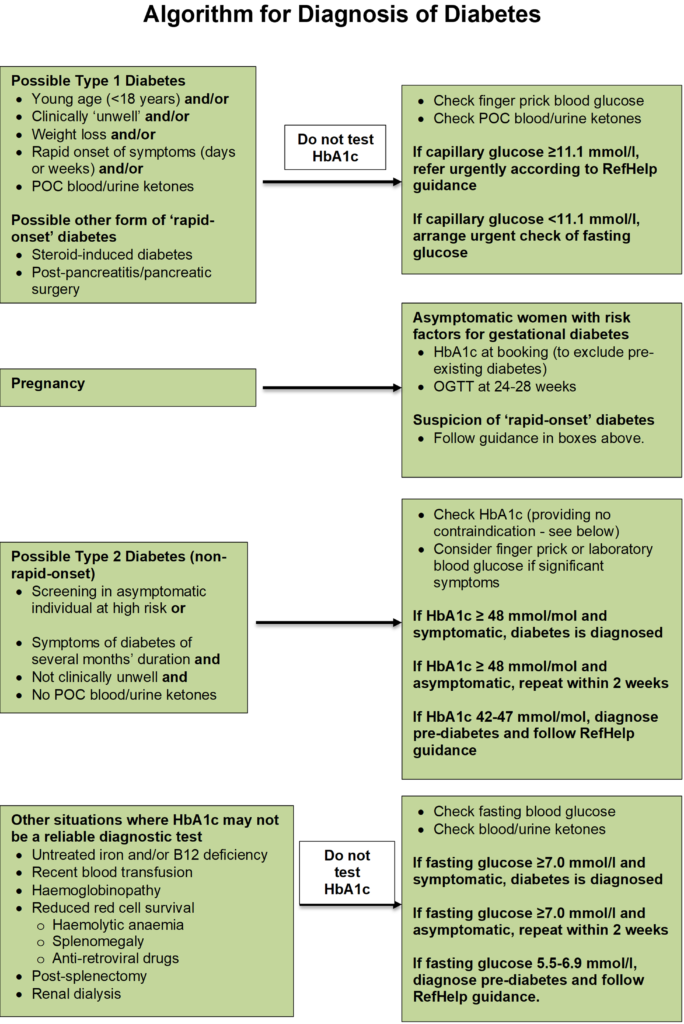
Which diagnostic test should I use?
There are pros and cons of each diagnostic test for diabetes. There are advantages of using HbA1c, because the patient does not need to fast, it is more reproducible than glucose, is easier to interpret (as you do not need to consider fasting/non-fasting status) and there is continuity in that this test will be used for monitoring purposes following a diagnosis of diabetes. However, there are situations when HbA1c must not be used as a diagnostic test (such as in children with suspected diabetes), as the results do not give an accurate measure of the diabetes status of the individual. These situations are shown in the accompanying algorithm.
Diagnostic HbA1c Testing in NHS Lothian
HbA1c is recommended as the diagnostic test of choice for non-rapid onset diabetes in NHS Lothian. The attached algorithm shows the situations when HbA1c should and should not be used. Guidance on referral criteria for people with newly diagnosed diabetes and pre-diabetes are available on RefHelp, as is detailed information on Haemoglobin variants and use of Fructosamine. It is strongly recommended that a urine or point of care (POC) finger-prick capillary blood sample is checked for ketones in all symptomatic people with suspected diabetes and in asymptomatic individuals subsequently diagnosed with diabetes.
Blood Ketone Testing
Blood ketone testing is a good alternative to urine ketone testing, particularly in dehydrated individuals who may struggle to provide a urine sample. It provides an immediate measure of ketone status from a capillary sample of blood. With increasing use of SGLT2 inhibitors for Type 2 diabetes, which are associated with a risk of euglycaemic ketoacidosis during intercurrent illness, the Lothian diabetes MCN advises that practices should consider getting a blood ketone meter/test strips for the assessment of unwell individuals on these agents.
Ketonaemia can clearly be an indicator of diabetic ketoacidosis, or incipient ketoacidosis. However, low level ketonaemia can be found in individuals who are fasting or who are following a low carbohydrate diet. Below is a guide for interpretation of blood ketones in someone with a new diagnosis of diabetes.
| Blood Ketones | Interpretation/Action |
| <0.6 mmol/l | Normal |
| 0.6-1.5 mmol/l | Possible incipient DKA. Phone on-call diabetes team |
| >1.5 mmol/l | High probability of DKA. Admit immediately to hospital if unwell. Otherwise phone on-call diabetes team |
There are 2 types of ketone strips listed as 1st choice on the formulary. The Nipro 4Sure beta-ketone testing strips and the Freestyle Optium beta-ketone testing strips; the former are half the price of the latter at £9.92 for 10 strips The compatible meter is the Nipro 4Sure Duo meter. These can be ordered by practices by emailing irene.jacobs@nipro-group.com or sales.support@nipro-group.com. Educational videos are available at: https://www.nipro-diagnostics.co.uk/educational-videos
Who to refer:
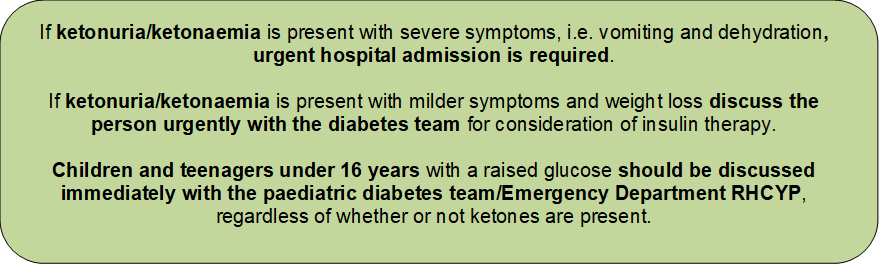
EMERGENCIES
Any possible NEW diagnosis of Type 1 Diabetes Mellitus is a medical emergency
- Hyperglycaemia (i.e. random glucose > 11.0 mmol/L and/or HbA1c > 48 mmol/mol)
- Rapid weight loss
- Systemic symptoms with a short prodrome
- Ketonuria
Any existing diabetes patient acutely unwell and at risk of DKA (see managing diabetes in acute illness)
Any suspected limb-threatening or life-threatening diabetes foot problem
- Ulceration with fever or any signs of sepsis
- Ulceration with limb ischaemia
- Clinical concern of deep-seated soft tissue or bone infection
- Gangrene
Any pregnant women with new diagnosis of diabetes with HbA1c – 48 mmol/mol OR fasting glucose – 7.0 mmol/L OR 2 Hours glucose – 11.1 mmol/L
For Adults Contact on-call Diabetes Registrar for either WGH or RIE via switchboard (0131 536 1000) or SJH by paging Diabetes Specialist Nurses (01506 523 000)
For children (under the age of 14) contact the paediatrics diabetes on-call register at the RHCYP via switchboard (0131 536 1000)
URGENT
- Antenatal diabetes
- Patients under the age of 40 with a new diagnosis of diabetes but not acutely unwell
- Patients with Type 2 Diabetes with suboptimal control, osmotic symptoms and weight loss necessitating insulin therapy
- All other patients with diabetes with a new foot ulcer (i.e. who do not have the emergency referral criteria as above)
ROUTINE
- New patients with established Type 1 Diabetes Mellitus requiring an unscheduled treatment review
- New patients with Type 2 Diabetes Mellitus under the age of 40
- Patient with Type 2 Diabetes not meeting HbA1c targets despite maximal tolerated oral agents
- Type 2 diabetes patients with chronic complications and suboptimal control
- Patients with diabetes complications requiring specialist input i.e. peripheral neuropathy, CKD
- Patients where the type of diabetes diagnosis is unclear
- All diabetes patients with suspected secondary diabetes or suspected MODY or family history of MODY
ADVICE only
- Uncertainty of diabetes diagnosis
- Patients starting oral drug therapy for steroid induced hyperglycaemia
- Optimisation of non-insulin drug therapies to improve HbA1c target
- Patients already attending secondary diabetes clinic
Who not to refer:
- Diabetes or Pre-diabetes patients requiring help with weight loss only:
- Diabetes patients can be referred for Tier 2 or Tier 3 weight management, the Counterweight Plus remission programme for Type 2 Diabetes or for bariatric surgery with following referral form on SCI-gateway (link) or patients can self-refer by emailing
weight.management@nhslothian.scot.nhs.uk
- Pre-diabetes patients can be referred for Type 2 Diabetes Prevention and Prediabetes education programme, Let’s Prevent to following email
weight.management@nhslothian.scot.nhs.uk
Alternatively, contact weight management team on 0130 537 9169 from Monday-Friday 9-5
- Diabetes patients under age of 14 see Paediatrics Endocrinology (LINK https://apps.nhslothian.scot/refhelp/Paediatric/PaediatricEndocrinology )
- Diabetes patients for retinal screening only see Diabetes Retinopathy (link to https://apps.nhslothian.scot/refhelp/Ophthalmology/DiabeticRetinopathy)
How to refer:
- Emergency referrals phone (see above to phone on call registrar) then complete Urgent SCI gateway referral through RIE/WGH/SJH/RHCYP-Diabetes
- General referrals: SCI Gateway through RIE/WGH/SJH/LCTC/RHCYP- diabetes
- Advice only New Referrals: SCI Gateway –RIE/WGH/SJH/ELCH/LCTC-diabetes-advice only
- Advice only existing patients Email:
St Johns Hospital Clinadvdiabetes@nhslothian.scot.nhs.uk
Western General Hospital WGH.DiabeticAdvice@nhslothian.scot.nhs.uk
Royal Infirmary Edinburgh RIE.DiabeticAdvice@nhslothian.scot.nhs.uk
The Email advice lines are useful for simple queries for patients whom you envisage to continue to manage in primary care. The advice emails are not appropriate for urgent referrals, which should either be sent in via SCI Gateway or discussed with the diabetes registrar on call.
The Email advice lines are not ideal for complex queries where the responding consultant would benefit from full past history and medication list; these patients should still be referred using the Advice Only option on SCI Gateway.
For specialty clinics see referral guidance under each section.
Useful information to include with your referral:
Recent HbA1c
Urinalysis for ketonuria
BMI
Acute diabetic symptoms such as rapid weight loss
Known diabetic complications
Blood pressure
PCR or ACR
Smoking status
Lipid profile
Link to Edinburgh Centre for Endocrinology and Diabetes (Lothians) http://www.edinburghdiabetes.com
link to My Diabetes My Way (Scotland) http://www.mydiabetesway.scot.nhs.uk/
link to diabetes UK https://www.diabetes.org.uk.
https://services.nhslothian.scot/diabetesservice/patient-information-leaflets/













