History
- Severe pain usually in a single joint
- Acute onset (typically less than 24 hours, often overnight) with episodes lasting 1 to 2 weeks
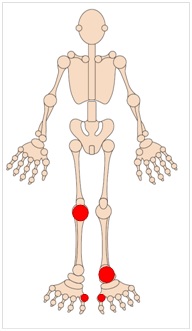
- Frequently involves 1st MTPJ, foot or ankle, but may involve any joint especially if coexistent osteoarthritis
Examination
- Tender, hot, red, swollen joint(s)
- Tophi appear as chalky white deposits and are markers of severe disease. Typically form in digits or over elbows.
Investigations
- Baseline renal and liver function
- Convalescent serum urate (4-6 weeks after attack)
- X-ray of symptomatic joints (characteristic erosions in established disease)
- Good practice recommends screening patients for cardiovascular risk factors
- Synovial aspirate usually not performed in primary care
M.A & H.B/S.R 25-01-24
A diagnosis of gout can be made in primary care using the following criteria. A score ≥ 8 gives at least an 80% likelihood of gout.
| Criteria | Score |
| Male sex | 2.0 |
| Previous reported arthritis attack | 2.0 |
| Onset within 1 day | 0.5 |
| Joint redness | 1.0 |
| First metatarsophalangeal joint involvement | 2.5 |
| Hypertension or ≥ 1 cardiovascular disease | 1.5 |
| Serum uric acid > 0.35 mmol/l | 3.5 |
Referral:
When to refer:
- Where there is suspicion of septic arthritis urgent referral is indicated for joint aspiration – contact oncall team
- Consider routine referral if there is diagnostic uncertainty. The differential diagnosis includes pseudo-gout secondary to chondrocalcinosis, and psoriatic arthritis.
- Genuine treatment resistance (noting that compliance with therapy is notoriously poor).
When not to refer:
Most patients with gout are managed in primary care.
Management
Please see separate flowcharts summarising Gout management and Prescribing for gout in renal impairment which has been recently updated.
The option of urate lowering treatment should be discussed with all patients in whom a diagnosis of gout has been made. Starting urate lowering treatment is often delayed until acute flares have resolved, however there is some evidence supporting initiation during acute flares.
To ensure clearance of urate crystals current guidelines recommend achieving serum urate levels below 0.3mmol/L in newly diagnosed patients and in those with tophi. For long term maintenance levels below 0.36mmol/L should be sufficient to prevent a recurrence of disease.
Urate lowering treatments
- Allopurinol is effective in the majority of patients. To reduce paradoxical flares we advise starting 100mg daily, and increasing at monthly intervals by 100mg until urate target is achieved. A median dose of 400mg daily was required to achieve target serum urate levels in a recent UK study, though with normal renal function doses up to 900mg daily (divided doses) can be used.
- Febuxostat is a second line xanthine oxidase inhibitor. Initially prescribed 80mg daily, the dose can be increased to 120mg daily if target serum urate not achieved.
- Sulphinpyrazone is licensed as an alternative or adjunct to allopurinol, however, supply problems mean that it is currently not possible to obtain.
- Benzbromarone is available on a named patient basis due to it being rare but serious hepatotoxicity. If you feel that a patient requires treatment with benzbromarone then please refer them to the gout clinic. Note that many patients opt to retry allopurinol after discussion of the issues around benzbromarone!
When should serum urate be measured?
When assessing the effectiveness of any given dose of urate lowering therapy it is advisable to wait for at least 2 weeks before measuring the serum urate.
- Serum urate can be misleading if measured during an acute attack of gout since up to 50% of patients will have normal levels due to a direct effect of inflammation on urate excretion. Current guidance suggests waiting 4-6 weeks after the acute presentation before measuring serum urate levels. If levels are measured during an acute attack be prepared to ignore the result!
- Most patients with a raised urate do not have gout so a diagnosis of gout cannot be made on the basis of the urate level alone. Similarly there is no justification for the use of urate lowering treatment in patients with isolated hyperuricaemia.
Flare prophylaxis
Flares of gout may continue for at least 12 months after urate control, and are paradoxically more common with aggressive urate lowering.
To reduce flares prophylaxis should be offered with continuous colchicine 500mcg b.d. for up to 6 months in all patients being considered for urate lowering therapy.
Patients with frequent flares and those starting on potent urate lowering therapy (ie Febuxostat) will benefit the most from the use of flare prophylaxis. Conversely patients with infrequent flares can simply be given a supply of emergency flare treatment with advice to take this as soon as a flare is experienced. Consider low dose NSAIDs in patients intolerant of colchicines
Doesn’t colchicine cause frequent GI side effects?
- Early colchicine treatment regimens with hourly dosing were associated with a high risk of GI side effects. Fortunately lower dose regimes have shown equal efficacy and are generally well tolerated. Current recommendations in acute gout are 500mcg BD, increased if tolerated and required to maximum QID.
If diarrhoea/colic occur, reduce colchicine to maximum tolerated dosage frequency.
For flare prophylaxis treatment with twice daily colchicine has been well tolerated for up to 6 months with no increase in adverse effects seen over placebo. In patients with severe renal impairment dose reduction is advised, with once daily colchicines still helpful.
What about drug interactions?
- Colchicine is contraindicated in patients with renal or hepatic impairment who are taking a P-glycoprotein inhibitor (e.g. cyclosporine, verapamil or quinidine) or a strong CYP3A4 inhibitor (e.g. ritonavir, atazanavir, indinavir, clarithromycin, telithromycin, itraconazole or ketoconazole).
Patients on a statin should be warned that there is an increased risk of muscle pain with this combination of treatments.
- Azathioprine is metabolised to 6-mercaptopurine which is inactivated by the action of xanthine oxidase. When 6-mercaptopurine or azathioprine is given concurrently with Allopurinol, only one-quarter of the usual dose of 6-mercaptopurine or azathioprine should be given because inhibition of xanthine oxidase will prolong their activity.
Although interaction studies with febuxostat have not been performed given its mechanism of action it is also likely to result in an increase in mercaptopurine or azathioprine levels, and concomitant use is similarly not recommended.
- For information on the other interactions with febuxostat, colchicine or allopurinol please refer to the current Summary of Product Characteristics http://www.medicines.org.uk/EMC/
Non-pharmacological
Where possible avoid, reduce or stop diuretics.
Reduce alcohol intake to within recommended limits.
Aim for ideal body weight by gradual weight loss.
Avoid sugar sweetened beverages and rich foods (liver, kidney, shellfish) and encourage skimmed milk and vegetable proteins.
Coffee has been shown to lower urate levels so can be encouraged.
Prescribing for Gout in Renal Impairment
BSR Guidelines on Gout (rheumatology.org.uk)
Patient information available on the Edrheum website













