COVID-19: Advice from the Scottish Government is changing frequently as different areas move into different levels of restriction. At some levels, there is advice regarding those who are shielding. The asthma team have taken the view that no children or young people under our care are in the category of extremely vulnerable, therefore we do not recommend shielding restrictions for any of our patients. If this advice changes we will contact the families affected.
Information
RHCYP
- Asthma clinic is held every Wednesday afternoon usually (Drs MacLeod and Gahleitner). It is a mixture of new patients and review patients. Respiratory Physiologists and Asthma Nurse Specialists support this service. (Julie Westwood and Ann McMurray) Children over 2 years of age with asthma or suspected asthma are seen at this clinic. Children are currently been seen predominantly on NHS Near Me with a small number being seen each week face to face.
- Critical Care Clinic is held on the last Wednesday of the month (Prof Cunningham). All children who have required high dependency or intensive care treatment will be seen there.
- Respiratory clinic is held every Tuesday afternoon (Drs Urquhart, Unger, Gahleitner McDougall, Armstrong and MacLeod) and Friday morning (Drs Armstrong and Urquhart) Children under 2 years of age with recurrent cough/wheeze or suspected asthma are seen at this clinic.
- Nurse Led Asthma clinic is also available every Friday morning. (Ann McMurray)
- Nurse Led Asthma Education clinic is held once per month on a Wednesday morning. (Julie Westwood)
- Adrenal Suppression service available to all children under 16 on above license doses or a high dose accumulation of inhaled, nasal or topical steroids (Julie Westwood)
- “Difficult asthma” discussion – monthly round-table professionals meeting about patients causing concern. Review of medical information, discussion of background information, MDT involvement. Primary care professionals are welcome to feed into this process.
St John’s Hospital
- Asthma clinic is held every alternate Thursday morning (Dr Rhodes). It is a mixture of new patients and review patients. A Respiratory Physiologist and an Asthma Nurse Specialist support this service. (Julie Westwood)
- Nurse Led Asthma Clinic is held once per month on a Monday afternoon. (Julie Westwood)
- Adrenal Suppression Service (as above) – Julie Westwood
- “Difficult Asthma” clinic is held 4 times a year. This is a joint clinic with a respiratory consultant from RHSC and Dr Rhodes and an Asthma Nurse Specialist (Julie Westwood)
Who to refer:
Asthma clinic
- >2 years of age
- Diagnosis unclear or in doubt (after a trial of treatment – email for advice asthmanurses.rhcyp@nhslothian.scot.nhs.uk
- Rapid escalation in treatment with poor response to treatment
- Excess use of bronchodilator therapy (despite adequate treatment and good adherence)
- Multiple courses of oral steroids (more than 2) in a year
- Regular requirement for inhaled corticosteroids above licensed doses
- High dependency/ Intensive care admission (if not already followed up by secondary care)
- Recurrent viral induced wheeze which requires oral steroids
- Significant Parental anxiety or need for reassurance
- Children with asthma and co-existing nut allergy/ previous anaphylaxis
Respiratory clinic (all BTS/ SIGN referral criteria)
- ≤2 years of age
- Symptoms present from birth or perinatal lung problem
- Excessive vomiting or posseting
- Persistent wet or productive cough
- Family history of unusual chest disease
- Failure to thrive
- Nasal polyps
- Unexpected clinical findings e.g. focal sounds, inspiratory stridor
Who not to refer:
- Mild intermittent, or mild to moderate persistent asthma, unless any features documented above
- Children under 2 years of age with viral induced wheeze (unless requiring regular courses of oral steroids/ hospital admission or frequent GP contacts)
- Children above 2 years of age achieving good control with short acting beta2 agonist and low dose inhaled corticosteroids (within license), combination therapy (within license), or leukotriene receptor antagonists.
- Children who have not received trial of treatment (email advice can be given if unsure)
How to refer:
Referrals should be made via SCI gateway however Dr MacLeod and Ann McMurray (Asthma Nurse) will answer queries via email. Please use internal email RHCYP, Asthma Nurses.
Referral letters do not need to be long however we would find it helpful to have an initial statement on reason for referral. A comment on wheeze heard on auscultation by a health care professional, treatments trialled, inhaler technique and adherence would be beneficial.
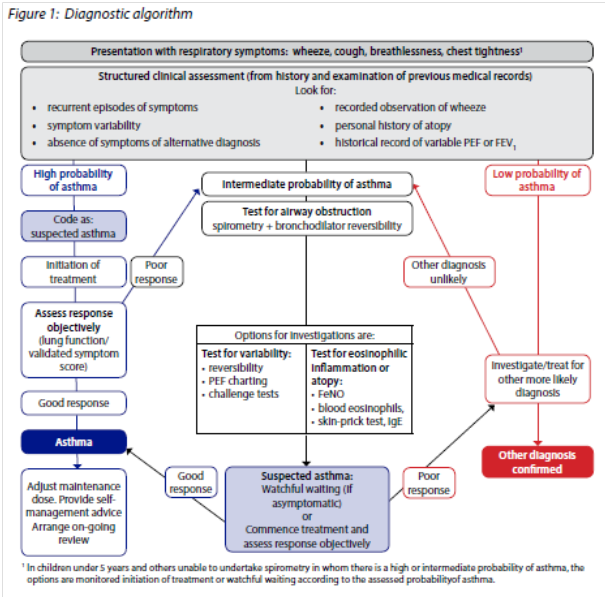
Paediatric asthma should be assessed and managed in accordance with the BTS/SIGN Asthma Guideline. We are aware there are some difference in approach compared with the most recent NICE guidance. To avoid confusion we recommend following BTS/SIGN guidance.
There is an expectation now that all children will be provided with a salbutamol inhaler and taught appropriate inhaler technique. Guidance is given on the initiation of inhaled steroids and appropriate dosage here http://www.ljf.scot.nhs.uk/LothianJointFormularies/Child/3.0/3.2/Pages/default.aspx
Management of an asthma attack.
The most common cause of an asthma attack in children is the common cold. Children and their families should be educated on the management of these episodes and be provided with an Asthma Action Plan Child Final Jan 2019.pdf with clear written instruction.
During colds, children should be encouraged to use their reliever inhaler 4 puffs, 4 times a day for 4 days. Should this dose be ineffective or limited (less than 4 hours) then children can have a multi dose (Salbutamol 100mcg pMDI – 10 puffs via a spacer) on one occasion. If this dose needs to be repeated within a 24 hour period the child should be medically reviewed – day or night.
A number of children (especially preschool) will have an acute wheeze attack without a diagnosis of asthma. Primary care assessment and management of acute wheeze in is the same as for older children, however attention should be paid to any child receiving multiple courses of oral steroids from whatever source (e.g. A&E, OOH, GP, clinic etc.). Such patients should be discussed early with the asthma team.
When to refer to hospital
- Symptoms persisting despite oral steroids and multidose Salbutamol*
- Oxygen Saturations <92% (please make sure you are using a weight appropriate probe for children)
- Child with any feature of a life threatening or a near fatal attack
*Parents are advised that it is unsafe to provide regular multidose Salbutamol at home in a child with an asthma attack. Parents are advised to provide a single multidose (10 puffs – 1 puff each minute for 10 minutes), and if that does work or if a further multidose is required within the next 24 hours then medical review is sought.
Requires emergency ambulance transfer
Referral threshold reduced if:
- Concerns re: adherence
- Single parent/social isolation
- Psychological problems/learning difficulties
- Prior history of near-fatal or brittle asthma
- Presentation at night
Management en-route to hospital
- Stay with patient until ambulance arrives
- Administer high doses of bronchodilator through a spacer or nebuliser driven by oxygen if spacer not available.
- Administer oral steroids http://www.ljf.scot.nhs.uk/LothianJointFormularies/Child/3.0/3.2/Pages/default.aspx
Inhaler technique
We recommend the use of a spacer with all inhaled medication for children and young people. The preferred spacer is the Aerochamber plus Flow-Vu. This poster will help with selection of the most appropriate spacer. aerochamber plus flow vu for children.pdf. These leaflets can be printed and given to parents or sent electronically. AeroChamber mouthpiece.pdf and AeroChamber mask.pdf
Asthma Action plans
All Children should be provided with an asthma action plan. A copy of the plan can be viewed/printed off here Action Plan Child Final Jan 2019.pdf
https://www.sign.ac.uk/media/1383/qrg158.pdf
https://www.sign.ac.uk/media/1386/sign158-summary-of-management-children.pdf
https://www.sign.ac.uk/media/1388/sign158-categorisation-of-inhaled-corticosteroids-children.pdf
https://www.sign.ac.uk/media/1384/sign158-diagnostic-algorithm.pdf













