People living with HIV (PLWH) can be managed through the Regional Infectious Diseases Unit (RIDU) at the Western General Hospital, or by Genito-Urinary Medicine at Chalmers Sexual Health Centre. Antiretroviral therapy is highly effective and well tolerated, and if treatment is established at an early stage, then the prognosis is excellent. All PLWH should be referred to a specialist centre for treatment and monitoring.
Provision of PrEP & PEPSE, and HPV vaccination for gay, bisexual and other men who have sex with men (GBMSM), can only currently be provided in Scotland through sexual health services.
Who to test:
HIV testing is recommended per NICE and the British HIV Association’s Adult HIV Testing Guidelines.
An HIV test should be offered to anyone who:
- Requests a test
- Has current or past risk factors for acquisition of HIV*
- Has another sexually transmitted infection
- Has an AIDS defining condition, an indicator condition, or clinical features of HIV infection: please see the HIV Indicator Conditions page for more detail.
*Groups at increased risk of exposure to HIV include:
- GBMSM
- Female sexual contacts of GBMSM
- Black Africans
- People reporting current or prior injecting drug use
- Sex workers
- Prisoners
- Trans women
- People from a country with a high HIV seroprevalence (>1%)
- People reporting sexual contact with anyone from a country with a high diagnosed seroprevalence, regardless of where contact occurs
- Individuals known to have/have had a mother living with HIV who do not have documented HIV-negative status.
Please see details of blood borne viruses more generally.
For guidance on where to start with assessment and testing for STIs and related conditions see STI and HIV – where to start.
GBMSM who require routine testing for STIs and HIV can be tested in general practice. Please see:
- MSM services for other services offering testing
- Details of testing in GBMSM
If you are not sure what testing is required more generally, or who to refer, please see STI testing and assessment.
Individuals should be made aware they are being tested for HIV and that testing is voluntary, and informed how their result will be managed. Lengthy pre-test discussion is not required. How much additional information is provided will vary to an extent based on the setting, the purpose of testing and the individual being offered a test.
If a person at risk chooses not to take up the offer of an HIV test, then they should be given advice on alternative nearby testing centres and how to access self-sampling kits. Information is available at NHS Inform (HIV symptoms & treatments – Illnesses & conditions | NHS inform).
Please see the BBV page for additional information on testing, referrals, primary care management and resources.
Test Details
The initial screen for HIV is performed on clotted blood (4.9mL brown capped gel tube); confirmatory testing will be requested by the laboratory for all positive HIV antigen/antibody tests to confirm patient identity.
For patients with poor venous access or needle phobia, dried blood spot (DBS) testing is also available – contact community BBV team at RIDU on 0131 537 2820 or email communitybbvteam@nhslothian.scot.nhs.uk.
C.M & N.B 06-02-24
Who to refer:
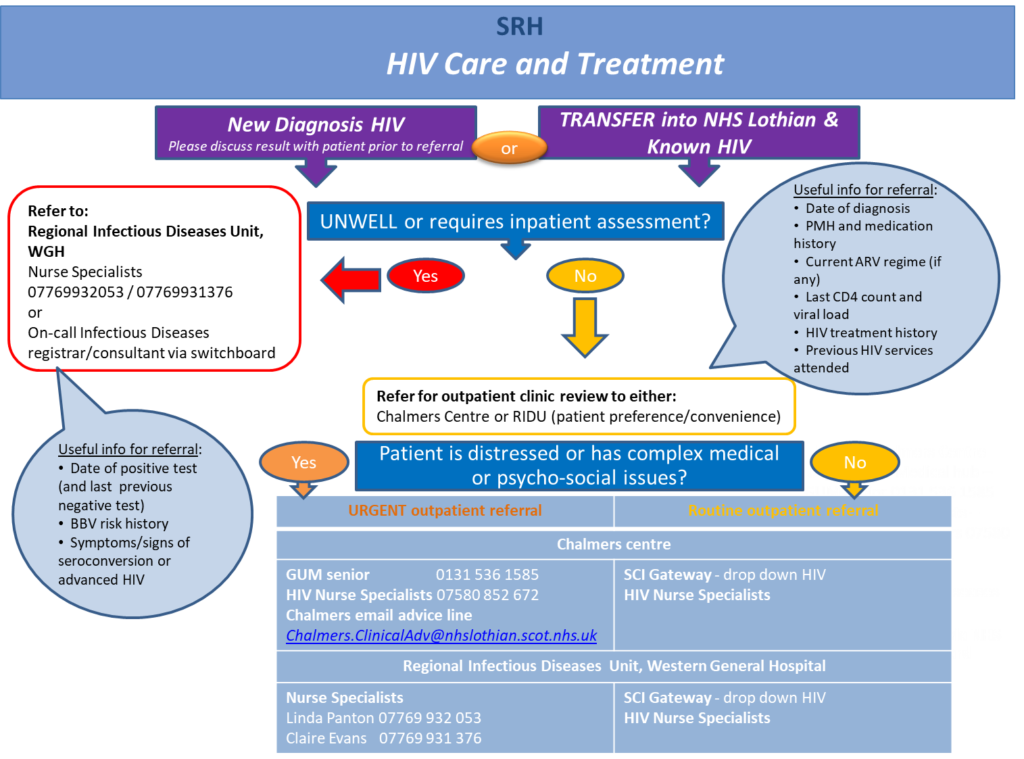
All patients who test positive for HIV antigen/antibody should be referred to RIDU or GUM treatment centres. Any clinician can make a referral. PLWH who are co-infected with viral hepatitis can be managed solely by RIDU or jointly by RIDU & GUM. Consider patient’s preference, location, and other services already involved/required.
Acutely unwell PLWH should be discussed with the on-call Infectious Diseases doctor for RIDU via WGH switchboard, as admission may be required.
Regional Infectious Diseases Unit (RIDU), WGH, Wards 41/42/43
Tel. 0131 537 2820/2823 (OPD Reception)
How to refer:
The on-call Infectious Diseases doctor can be contacted directly for advice, urgent clinic appointments and admissions – page via WGH switchboard 0131 537 1000.
Newly diagnosed but asymptomatic PLWH should be referred urgently for outpatient assessment via SCI Gateway ‘Infectious Diseases’ or by letter to RIDU.
The HIV Clinical Nurse Specialists are also able to provide advice and arrange follow up for PLWH known to RIDU, those transferring HIV care and newly diagnosed but asymptomatic individuals. Please contact 0131 537 2959 between 8am – 5pm to discuss. There is also an option to leave a message.
Genito-Urinary Medicine at Chalmers Sexual Health Centre
Tel. 0131 536 1070
Chalmers is a specialist outpatient centre for HIV and sexual health. Please see the Sexual and Reproductive Health pages on RefHelp for further information.
How to refer:
Please see the Sexual Health Guidance on ‘What to Refer and How’
- SCI gateway ‘Sexual and Reproductive Health and GU Medicine’
- New referrals can be made by letter or by telephone to the GUM consultant on call
- Telephone 0131 536 1585 or via the RIE switchboard Monday-Friday 9.00am-5.00pm
- Letter to Department of Genito-Urinary Medicine
- An email advice service for healthcare professionals is also available (Chalmers.ClinicalAdv@nhslothian.scot.nhs.uk)
PLWH who decline referral to specialist services should be encouraged to accept referral to a specialist centre, with the offer repeated opportunistically whenever possible.
GPs may wish to consider sending a 2.6mL red capped EDTA tube to Haematology for a CD4 cell count and contacting Infectious Diseases, who will advise as to whether prophylaxis against opportunistic infection should be offered.
Patients should be offered screening for other BBV infections, such as HBV and HCV.
https://www.nice.org.uk/guidance/qs157/chapter/quality-statement-3-hiv-indicator-conditions
https://www.bhiva.org/HIV-testing-guidelines
Asymptomatic HIV infection | Diagnosis | HIV infection and AIDS | CKS | NICE
HIV symptoms & treatments – Illnesses & conditions | NHS inform
Primary Prophylaxis of OIs — EACS Guidelines (sanfordguide.com)














