Chronic rhinosinusitis is a chronic disease requiring ongoing long-term medical management: the ideal is for optimal, prolonged therapy to reduce inflammatory components prior to considering referral. Please see Primary Care Management for full details.
Referrals for septal deformities or deviations are accepted where there is significant airway obstruction. However, patients need to be informed that there will be a long waiting time for assessment and surgery (up to 2 years).
Sinonasal Cancers.
The Scottish Referral Guidelines for Suspected Cancer emphasise that sinonasal cancers are rare, whilst benign rhinosinusitis symptoms are common.
The associated clinical features include progressive or new unilateral nasal obstruction with one or more of:
- Proptosis
- Epistaxis
- Dental pain or loosening dentures
- Cranial nerve palsy or nasal (not facial) pain.
However, sinus and nasal symptoms are common presenting features in primary care and are frequently benign (e.g. rhinosinusitis or benign nasal polyps). If there is concern that there is a nasal or paranasal cancer, please refer via the USC pathway.
Rhinitis.
Rhinitis is inflammation of the nasal mucosa. Clinically it is defined as 2 or more of the following symptoms for more than 1 hour on most days:
- Nasal discharge
- Nasal obstruction
- Sneezing/Irritation
The East Region Formulary outlines principles of treatment, including the need in some for prolonged and combination treatment.
C.M. & A.H. – 10/2/26
Who to refer
Refer as USC where suspicion of a nasal or paranasal cancer (see sinonasal cancer above).
Referrals are also accepted for:
- Skin prick testing for allergy
- Failure of medical therapy (1st and 2nd line OR as per previous ENT recommendations) for recurrent acute sinusitis or chronic rhinosinusitis – see Primary Care Management for full detail.
- Structural deformity
- Persistent unilateral symptoms particularly if associated with serosanguinous discharge or facial pain
- Unilateral polyp or mass
History
Symptoms as above. Seek out other respiratory disease such as asthma. Check occupation (exposure to inhaled irritants), history of allergies/atopy, drug and smoking history.
Examination
Assess any obvious nasal deformity. Objectively assess airflow (condensation on cold metal or mirror). Perform anterior rhinoscopy and look for septal deviation, enlarged turbinates, nasal discharge and other unusual pathology such as polyps or tumours.
Investigation
If allergy is suspected and this diagnosis is going to change management, IgE screen (in primary care) or preferably skin prick tests (can be undertaken after referral to ENT). Patients must stop antihistamines at least 72 hours before skin prick testing.
Differential diagnosis
- Rhinosinusitis
- Structural obstruction
- Nasal hyperactivity
- Hormonal
- Drug induced
- Cancer (very rare)
Management
Primarily medical therapy using the least aggressive combination that gives symptom control.
- Regular saline nasal douching ( Please see leaflet on Salt Water Rinse).
- Allergen avoidance
- Antihistamine (if allergy suspected) also leukotriene antagonists may be considered in asthmatics
- Topical nasal steroid sprays (Minimum 2 bottle trial of first and second line before referral to secondary care)
- Systemic steroids (Prednisolone 25 mg a day for 2 weeks, only, is an option for all forms of Rhinitis)
- See the East Regional Formulary for recommendations for:
– Sinusitis
– Rhinitis
– Nasal Polyps
Treatment of Allergic Rhinitis
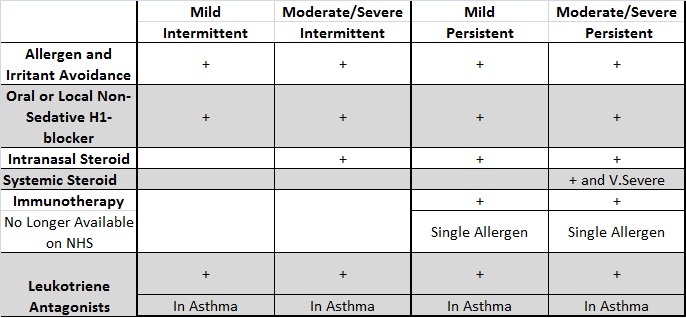
Effects of Medication on Symptoms
| Nasal Preparation | Sneezing | Itching | Rhinorrhoea | Congestion |
| Antihistamines | +++++ | ++++ | +++ | 0 |
| Anticholinergics | 0 | 0 | +++++ | 0 |
| Topical Steroid | +++++ | +++++ | +++ | +++ |
| Decongestant | 0 | 0 | + | +++++ |
| Mass cell stabiliser | +++++ | +++ | + | 0 |
| Leukotriene Antagonists | +++ | ++ | 0 | ++++ |
Hayfever NHS Choices – note that immunotherapy is not available under NHS care in Scotland.
Managing Hayfever and Pollen: ENT UK patient information leaflet













