Services
The Urogynaecology Department offers complete clinical and urodynamic assessment of female patients with pelvic floor dysfunction including lower urinary tract symptoms (LUTS) and incontinence, access to the nurse urogynaecology unit as well as surgical intervention for urinary incontinence and prolapse.
06-07-21
Who to refer:
Women with symptoms as above and:
- Failed Conservative Management
- Significant (beyond introitus) and / or Symptomatic Prolapse
- Previous Incontinence / Prolapse Surgery
- Previous Pelvic Irradiation
- Complicated symptoms (consider referral to urology):
- Haematuria
- Bladder pain
- Recurrent UTIs
- Difficulty with bladder emptying / Urinary Retention
- Suspected fistula
Women with a suspected pelvic mass should be first referred for an Ultrasound Scan to establish a diagnosis and then referred according to the findings.
If symptoms are of sudden onset or atypical, especially in the elderly, bladder malignancy should be considered with early referral urology.
Who not to refer:
- Women with uncomplicated symptoms who have not undergone initial primary care management
- Women with urinary symptoms due to a pelvic mass – this needs urgent investigation first (Ultrasound Scan)
- Women requiring input from physiotherapy – please refer directly to generic physiotherapy via SCI Gateway: this is the first line management for all those with any element of stress incontinence (SCI Gateway -AHP-Physiotherapy)
How to refer:
Via SCI Gateway: Specialty Gynaecology – Urogynaecology
Referrals Pathway to Women’s Health Physiotherapists in the Community across Edinburgh &Lothians (West/Mid/East)via SCI Gateway – Options:
AHP – Physiotherapy. Edinburgh – Community MSK HUB (Slateford)
AHP – Physiotherapy. East Lothian – East Lothian Community Hospital Please note – patients can self refer using form
AHP – Physiotherapy. Midlothian – Bonnyrigg Health Centre Please note – patients can self refer using form
AHP – Physiotherapy. West Lothian -St Johns Hospital
- Referrals will be directed to one of the Community Physiotherapy Services MSK Outpatient Clinics.
- Referrals will be triaged appropriately to a Women’s Health Physiotherapist.
PRESCRIBING FOR THE TREATMENT OF OVERACTIVE BLADDER IN LOTHIAN
Symptoms of overactive bladder include:
Urinary frequency / urgency / nocturia with or without urge incontinence
PRIOR TO PRESCRIBING MEDICATION:
1. Exclusion of the following:
- Haematuria
- Recurrent urinary tract infection
- Difficulty with bladder emptying
Any of the above and previous surgery for incontinence warrant early referral
2. Conservative management:
- Advice regarding fluid intake
- Bladder retraining
MEDICATION FOR THE OVERACTIVE BLADDER:
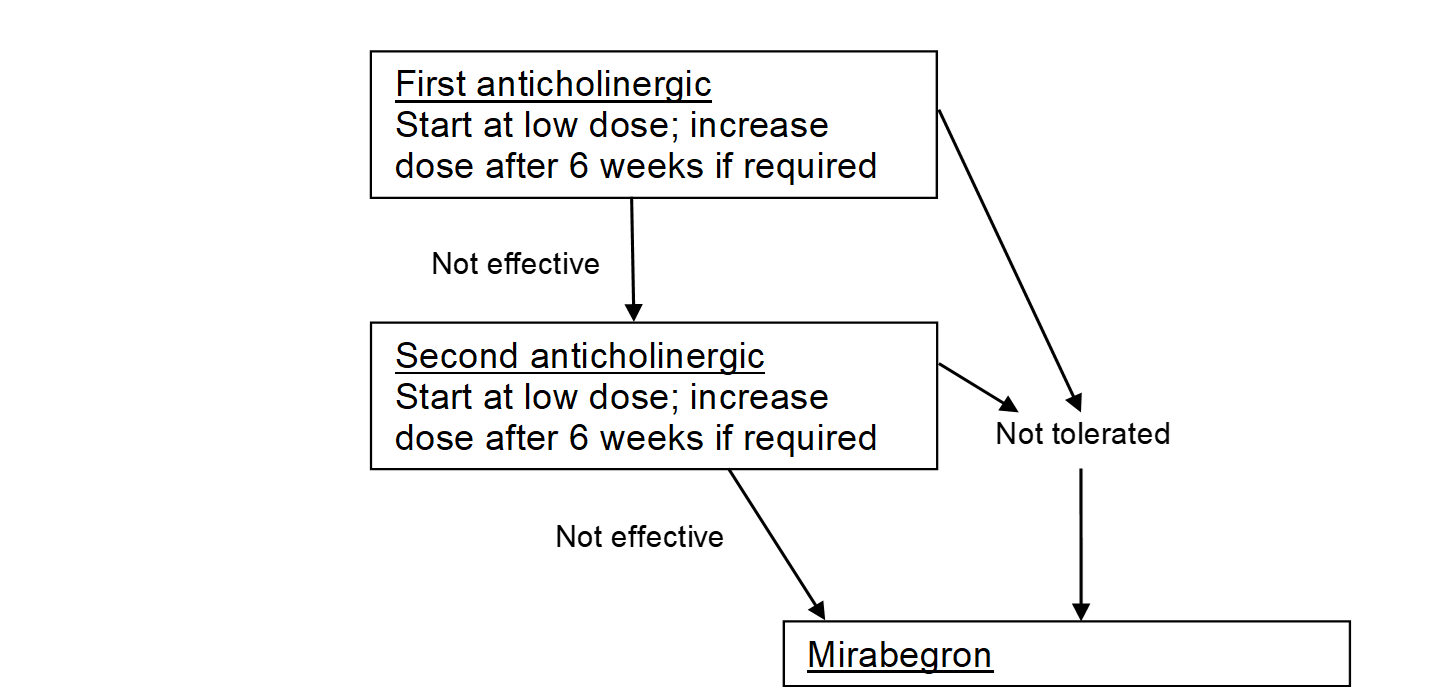
- Medication should be commenced at the lowest dose and titrated up as required and tolerated.
- If medication is not effective or not tolerated, the formulation should be changed.
- The use of medication for overactive bladder may be limited by side effects. These may be reduced by adjusting the dose or changing the formulation / application.
Generic antimuscarinic formulations:
Tolterodine tartrate (Tablets 1mg, 2mg)
Dose: 2mg twice daily. Reduced if not tolerated to 1mg twice dailyModified release tablets 4mg once daily
- Oxybutynin hydrochloride is no longer on the Lothian Formulary but is the only formulation available for transdermal application if oral application is not tolerated; it should not be used in patients aged over 65 due to increased risk of cognitive impairment
M3 selective antimuscarinic formulations:
Solifenacin (Tablets 5mg, 10mg)
Dose: 5mg once daily. Increase to 10mg daily if required
Fesoterodine (Tablets 4mg, 8mg)
Dose: 4mg once daily. Increase to 8mg daily if required
b3 Receptor agonist:
Mirabegron (Tablets 50mg)
Dose: 50mg once daily
- If antimuscarinic formulations are contra-indicated, not effective in controlling symptoms or not tolerated, the b3-receptor agonist is an alternative option.
- In patients who are already on medication with a high anticholinergic load, the b3-receptor agonist may be considered as a first line option.
- The lower dose of Mirabegron 25mg is available for patients with renal or hepatic impairment.
Pelvic health, Continence and Prolapse education video: https://vimeo.com/428502146
POGP-PelvicFloor Exercises for women
UK Pessary Guideline final April21
Management of Female Urinary Symptoms Printable Jan2020
Guidance on use of BASICS community assessment of bladder function
Physiotherapy Pelvic Floor Urinary incontinence Prolapse














