Possible differentials include: posterior vitreous detachment (PVD), retinal detachment, vitreous haemorrhage, retinal tear or holes.
Patients with sudden onset flashes and floaters require a dilated fundoscopy examination. This can be carried out by an experienced optometrist.
If there is any suspicion of retinal detachment from examination or the history e.g. curtain over vision/shadow over vision refer as a suspected retinal detachment.
A PVD is where the vitreous changes in consistency and pulls away from the retina. It can lead to flashes and floaters and is commoner in increasing age. There is a small risk following a PVD of patients going on to develop a retinal tear/hole/detachment so every patient with a PVD should be given specific advice. They should watch out for worsening floaters/flashes and decreased vision/curtains over their visual field.
Risk factors for retinal detachments include recent cataract/retinal surgery, previous retinal detachment/hole/tear, PVD and myopia.
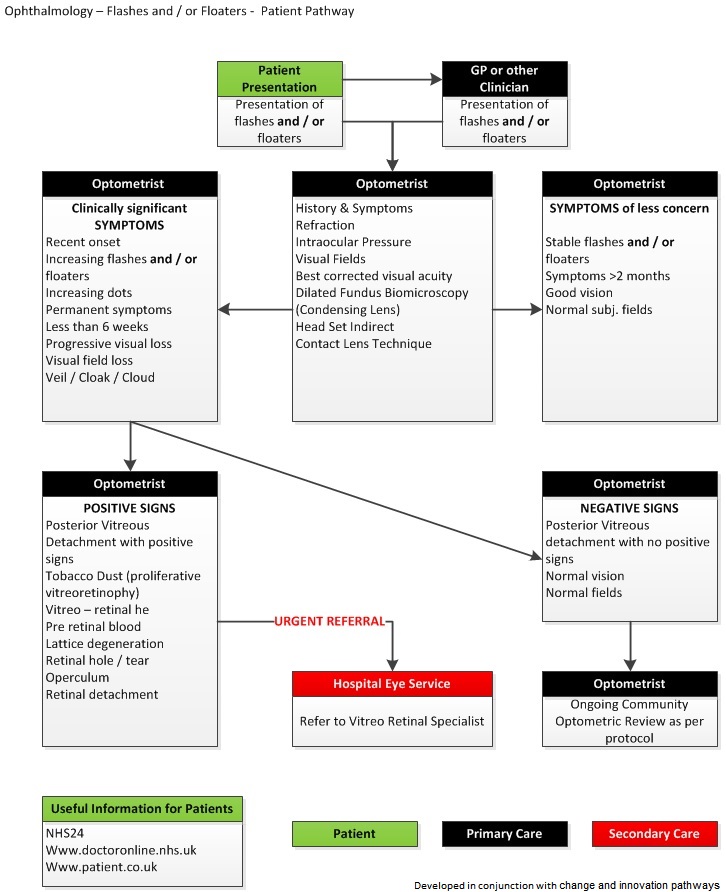
Ophthalmology – Flashes and Floaters – Guidance Notes
1. All patients presenting with symptoms of flashes and / or floaters should have a full history taken. One would be concerned if the symptoms are of recent onset, increasing and permanent.
All appropriate tests should be carried out to determine if there is any sight threatening disease present. This would include refraction, applanation tonometry, visual field assessment if possible, dilated indirect fundus biomicroscopy using a Volk type condensing lens or preferably a contact lens. An alternative method would be to use the indirect headset technique.
Certain clinical signs would warrant an urgent referral:
- Tobacco Dust
- Vitreous, retinal or pre-retinal haemorrhage
- Lattice degeneration with retinal break
- Retinal hole or tear
- Operculum – free or attached
- Retinal detachment.
2. The incidence of retinal breaks in patients aged 10 years or more who do not have any history of ocular disease is 6-14%. The incidence of retinal detachment is approximately 12/100,000 of the general population per year. This suggests that less than 0.2% of people with a retinal break eventually have a detachment of the retina. Only a minority of retinal breaks will go on to cause a retinal detachment. Posterior Vitreous Detachment does not have any harmful effect on pre-existing retinal breaks. All patients presenting with posterior vitreous detachment, no vitreous pigment, and no retinal tears or holes at initial examination can be safely discharged with an explanation of the warning symptoms which should prompt the patient to re-attend.
3. All patients presenting with a new onset of flashes and / or floaters should, if possible, undergo a dilated fundoscopy ideally by Volk lens. Patients should e questioned about the presence of a subjective visual field defect and if they notice one they should be referred to Eye Casualty or similar. The presence of pigment in the vitreous in patients with new symptoms is an indication for immediate hospital referral to Eye Casualty or similar, as is the presence of a vitreous haemorrhage. All patients should be counselled that if they should develop a visual field defect they should attend Eye Casualty or similar.
4. Where there is no sign of sight threatening retinal disease and the condition appears stable ongoing monitoring should take place in the community by the optometrist. The patient should be well advised of the symptoms of retinal detachment and to return for an examination should there be any concern.
In the absence of symptoms any nominal review period should be based on the time since symptoms last presented.
- Recent onset – recall 2 – 3 months
- 3 months – recall 6 months
- 1 year – recall annually
5. When signs and / or symptoms are present that indicate sight threatening disease the patient should be directly and urgently referred to a vitreo-retinal specialist for further investigation with a full, detailed report of the findings.
Who to refer:
Please see Lothian GP and optometry ophthalmology referral pathway.
Urgency of the condition for details on how soon patients should receive an appointment.
Patients who present with a problem with their only seeing eye should be advised to see an optician/ophthalmologist for review.
Who not to refer:
Consider getting an assessment by an experienced optometrist. Optometrists can provide appointments for patients as part of the General Ophthalmic Services Contract and are required to see emergency patients in a timely manner.
How to refer:
We require a referral letter for EVERY patient.
The preferred referral process is via SCI Gateway. If sending/forwarding a referral via SCI gateway please include past medical history, allergies and medications
If you do not have access to fax or SCI Gateway e.g. if you have arranged an appointment out of hours please send a written referral letter with the patient to bring to their appointment.
Only if SCI Gateway is unavailable should a letter be typed or handwritten. Please write legibly and include your examination findings.
If you have arranged an appointment in the acute referral clinic and you are referring from within another hospital in Lothian please use TRAK to type the referral letter.













