Information
Constipation in children
- Early intervention with oral laxatives in addition to non-pharmacological management is crucial to prevent chronicity, overstretched bowels with reduced motility, withholding behaviours and overflow soiling
- Affects 1 in 3 children; 95% cases are idiopathic with no pathological cause.
- Most patients with constipation can be managed in primary care.
- This RefHelp page can be used to guide assessment and need for referral.
- We are happy to see any child if there are concerns even if they strictly fall out with the referral criteria. These children should be referred to medical paediatrics; GI only see more complex patients.
Dyschezia is the term given to the apparent discomfort infants can experience prior to passing stool. It can often be mistaken for constipation but is managed differently. Please see this helpful PIL for parents: Dyschezia in babies v1.0.pdf
D.R.M & M.B. 25-11-24
Who to refer:
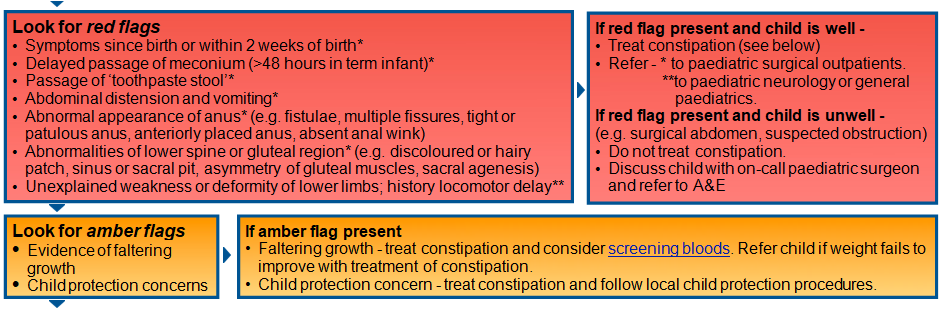
1. Any child with a ‘red’ or ‘amber’ flag according to the NHS Lothian constipation guidelines i.e: Guidelines-for-management-of-idiopathic-childhood-constipation.pdf
Screening bloods for children with suspected non-idiopathic constipation mentioned above:
- Full blood count
- Urea and electrolytes
- Liver function tests
- Calcium
- Thyroid function tests
- Coeliac screen (if gluten exposed)
2. Any child with chronic constipation not responding to recommended doses of laxatives (see Primary Care Management tab)
- Refer children < 1yr after 4 weeks optimal treatment.
- Refer children >1yr after 3 months optimal treatment.
3. Any child with faecal impaction +/- overflow who fails to respond to disimpaction regimens (see Primary Care Management tab)
- These children should be discussed with on-call paediatric team (link to urgent telephone advice main page) regarding possible admission for supervised inpatient disimpaction.
4. If you wish to refer a child who falls out with the above criteria, please state reason for referral.
Useful additional information for GPs and families
Diet
- Milk – too much milk can cause constipation, affect appetite, and cause iron deficiency anaemia.
- Over 1 year: aim to reduce intake to 400ml maximum/day (plus dairy in diet).
- Switching from a bottle to a sippy cup often leads to reduced intake, dilute milk if necessary.
- Fluid intake – aim for at least 5 drinks of water per day; more specific volume guide https://cks.nice.org.uk/topics/constipation-in-children/management/management/#recommended-fluid-intake
- Diet – increase fruit, vegetables, fibre.
Laxatives
Disimpaction (see Disimpaction-regimens.pdf for treatment regimen)
- Any child being disimpacted should be reviewed 1 week after treatment to ensure disimpaction successful and taking adequate maintenance therapy.
- Macrogol (Movicol/Laxido) can be difficult to get a child to take more than a few sachets per day due to high volumes required. Consider using Sodium Picosulphate (only needed for 2-3 days and easier to give).
- Abdo cramps are a common side effect of disimpaction treatment – do mention to parents – can treat with paracetamol, if concerns/abdo pain severe/concerned about child seek medical advice.
- If soiling, likely to be impacted – disimpact and start maintenance laxatives then review after 1 week.
Maintenance treatment (see Maintenance-Laxative-Therapy.pdf for treatment regimen)
- Always start on maintenance therapy immediately after disimpaction.
- Aim for one or two soft stools (type 3-4) most days.
- Children may require many months of maintenance treatment.
- Consider combination laxatives:
- If stool still too hard on one laxative, consider adding in a softener.
- If stool frequency too low on one laxative, consider adding in a stimulant.
- Softener/stimulant:
- Macrogols are combined softener and stimulant laxatives.
- Softeners: Lactulose, liquid Paraffin.
- Stimulants: Sodium Picosulphate; Senna; Bisacodyl; Docusate.
- Lactulose – can cause tooth decay – make a note on script – give before brushing teeth.
- Stopping laxatives – once stable for a period of time can trial off laxatives but wean off slowly (particularly if have been on for a long time), low threshold to restart / use on an as required basis.
- Macrogol (Movicol/Laxido) more palatable when chilled in the fridge, can be mixed with any fluid the child will drink (milk, squash)
Toileting behaviour
- Toileting – encourage sitting on the toilet/potty for short periods after meals e.g. to sit for 10 minutes shortly (5-10 minutes) after meals (at least once per day).
- Avoid punitive measures – constipation is not the child’s fault & punitive measures can make things worse
- Positive reinforcement – of good behaviours (rather than success which leads to despondency & disengagement) helps to establish regular bowel habit
Information for GPs
Constipation guideline NHS Lothian – https://apps.nhslothian.scot/files/sites/2/Guidelines-for-Management-of-Idiopathic-Childhood-Constipation.pdf
Bristol stool chart https://eric.org.uk/poo-checker/
Lothian Joint Formulary Child chronic constipation; faecal impaction https://formulary.nhs.scot/east/gastro-intestinal-system/colonic-disorders/constipation/
Clinical knowledge summary The Managment of Idiopathic Constipation in Children https://cks.nice.org.uk/topics/constipation-in-children/management/management/#overview-of-management
Information for Parents
Videos for parents – eric (resources in constipation section) or youtube Constipation – YouTube
ERIC – https://eric.org.uk/childrens-bowels/constipation-in-children/ on this link, click resources, there are several PILs that can be printed including ‘a parents’ guide to disimpaction’ and ‘how to use macrogol laxatives’
Eric – advice on toilet anxiety for parents – Toilet anxiety and toilet phobia in children – ERIC
Poo diary – can print and give to take home prior to next review https://eric.org.uk/wp-content/uploads/2022/08/poodiary.pdf
Constipation in children general information for parents which includes links to information on diet https://www.nhs.uk/conditions/baby/health/constipation-in-children/
Info on fibre (link on above website page) https://www.nhs.uk/live-well/eat-well/digestive-health/how-to-get-more-fibre-into-your-diet/
Please see this helpful PIL for parents: Dyschezia in babies v1.0.pdf













