Prolactin Measurement in Adults
Prolactin is produced by lactotrophs in the pituitary gland. Its biological function is to induce and maintain lactation in breast tissue for breast feeding.
Prolactin can be easily measured in serum and references ranges for men and women are calculated from the healthy population. In modern assays ‘macroprolactin’ (autoimmunity to prolactin causing a spurious hyperprolactinaemia) is routinely analysed in repeatedly elevated samples and reported. In these cases, the ‘monomeric’ result should be used.
Physiologically, lactotrophs are ‘kept in check’ by dopaminergic neurones from the hypothalamus which suppress prolactin production out-with periods of breast-feeding requirement. Therefore, any interruption of this process will increase prolactin levels.
Common causes of elevated prolactin are as follows:
1. Physiological
– Coitus
– Exercise
– Lactation
– Stimulation of nipples (including checking for galactorrhoea)
– Pregnancy
– Stress- emotional and physiological
2.Drug induced – common – non exhaustive list (common drug culprits)
– Oral contraceptives (not including progesterone only preparations)
– Antipsychotics (phenothiazines, risperidone, haloperidol, olanzapine, amisulpiride, clozapine, quetiapine)
– Antiemetics (metoclopramide, domperidone, prochlorperazine)
– Antidepressants (tricyclic antidepressants, SSRIs, monoaminoxidase inhibitors, SNRIs e.g. venlafaxine)
– Antihypertensives (verapamil)
– Antihistamines (H2 receptor blockers)
– Opiates
3.Pituitary pathology
– Pituitary prolactinoma or mixed secreting pituitary tumour
– Hypothalamic-pituitary stalk damage (other pituitary or external mass, trauma, surgery)
4.Systemic disorders
–Chronic kidney disease
– Hepatic cirrhosis
– Seizures
– PCOS
– Chest wall irritation – trauma, shingles, surgery
INDICATIONS FOR MEASURING PROLACTIN
Measuring prolactin levels without indication incurs significant cost due to unnecessary investigation as well as unnecessarily increasing patient concern. Examples in which prolactin is often measured without clear indication are headache, heavy menstrual bleeding and irregular periods (without oligomenorrhoea).
Clinical indications for measurement of prolactin in adults are:
- Persistent oligomenorrhoea over 12-month period (> 35 days between cycles) – NOT heavy menstrual bleeding/menstrual irregularity
- Primary or secondary infertility
- Primary or secondary amenorrhoea* (see below for definition)
- Galactorrhea (> 12 months from breast feeding or pregnancy)
- Pituitary mass on cross sectional imaging
- Secondary hypogonadism (low/normal LH and FSH with low Testosterone (male) or oestradiol (female)
- Genetic syndrome in which screening for prolactinoma is required
- Biochemical picture of Hypopituitarism (low TSH + Low t4, diabetes insipidus, growth hormone deficiency, secondary adrenal insufficiency)
- Gynaecomastia in the absence of other clear cause (obesity, elderly, puberty)
- New visual disturbance typical of chiasmic compression where pituitary mass is suspected.
*Primary amenorrhoea is defined as the failure to establish menstruation by 15 years of age in girls with normal secondary sexual characteristics (such as breast development), or by 13 years of age in girls with no secondary sexual characteristics.
*Secondary amenorrhoea is defined as the cessation of menstruation for 3–6 months in women with previously normal and regular menses, or for 6–12 months in women with previous oligomenorrhoea.
ML & CM 18/12/25
Who to refer
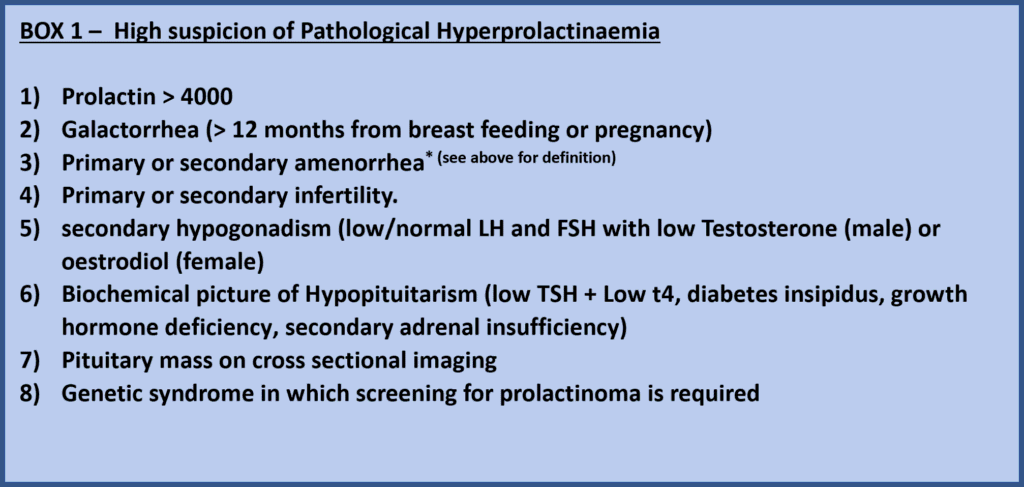
Anyone with a high suspicion of pathological hyperprolactinaemia:
- Prolactin > 4000
- Galactorrhea (> 12 months from breast feeding or pregnancy)
- Primary or secondary amenorrhea* (see above for definition)
- Primary or secondary infertility
- secondary hypogonadism (low/normal LH and FSH with low Testosterone (male) or oestrodiol (female)
- Biochemical picture of Hypopituitarism (low TSH + Low t4, diabetes insipidus, growth hormone deficiency, secondary adrenal insufficiency)
- Pituitary mass on cross sectional imaging
- Genetic syndrome in which screening for prolactinoma is required.
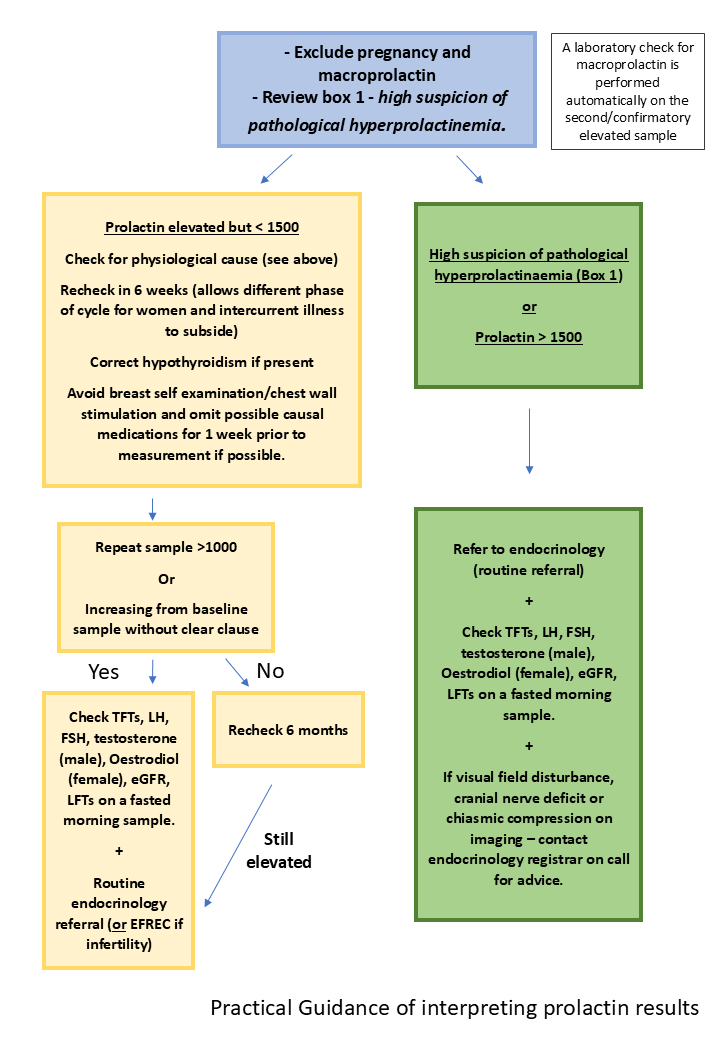
Those with a prolactin >1500 or a prolactin >1000 on repeat testing at 6m once other causes excluded (see flow chart above).
Who not to refer
- Macroprolactin positive results with a normal ‘monomeric’ result.
- Transient elevated prolactin which settles on repeat sample.
How to refer
By SCI Gateway to endocrinology at RIE or WGH – please note the option for advice only.













