(Patients having issues after initial management)
Information
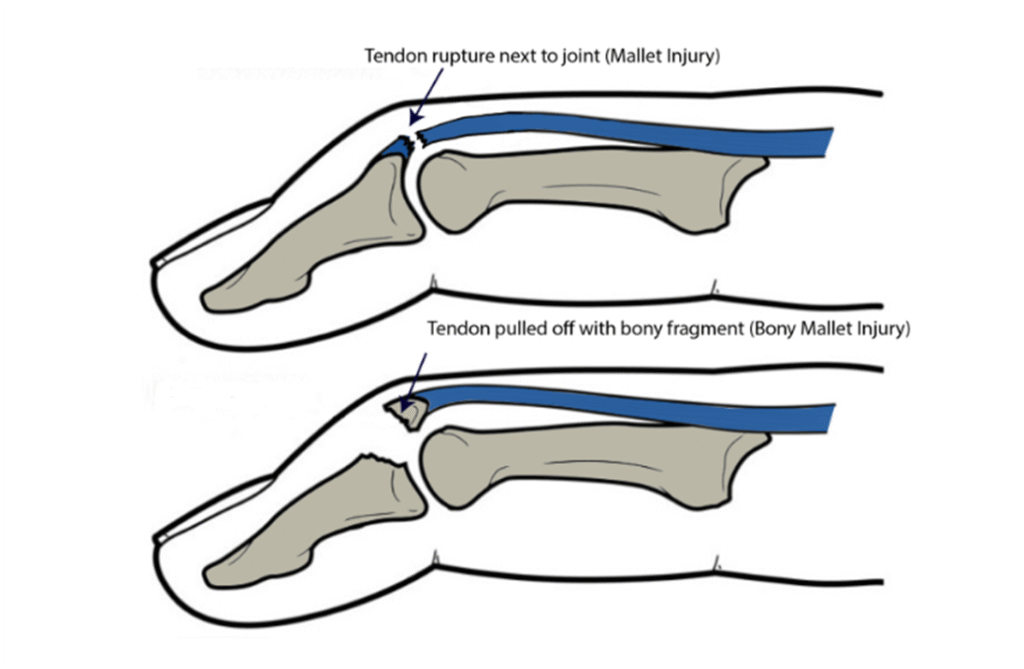
Mallet finger injury is an injury that occurs at the Distal Interphalangeal Joint (DIPJ) of the finger. It can be the result of the tendon pulling off the bone (tendinous) or secondary to a fracture of the distal phalanx at the joint (bony).
The result of the injury is that the patient is unable to straighten the end of their finger, and it droops.
Many patients will have attended the urgent care services for early management of their injury. If patients are attending primary care with an acute mallet injury, an XRay examination is recommended to determine whether the injury is tendinous or bony. If bony, then the size of the fragment may affect how the injury is managed with a very small proportion of patients being offered surgery.
Some patients may have been seen in the hand trauma clinic at St John’s Hospital. However, most patients in the Edinburgh area are managed via the Orthopaedic Trauma Triage Clinic (TTC) and are sent written information guidance rather than a clinic appointment.
Patients may attend their GP with ongoing concerns about the end of the digit continuing to droop despite proper use of their splint for the prescribed duration.
This guidance applies to those patients
Continuing deformity of the DIPJ after mallet finger injury management:
It is normal for the patient to notice the DIPJ continues to droop after treatment with a mallet splint. This is because the tendon/bone never goes to sit exactly back where it came from. This results in slack in the extensor mechanism, and therefore an extensor lag.
The finger may be straight when it first comes out of the splint but can droop within a few hours to a few days. It is normal and acceptable for the patient to have up to a 30-degree extensor lag at the DIPJ.
If the degree of extensor lag is >30 degrees, patients have the option of re-splinting the finger straight for a further 6-8 weeks, but there is no guarantee that the finger will end up in a better position in the long term. In fact, it is likely that the finger will be stiffer due to prolonged splintage in extension.
The hand functions better with finger flexion, so an extensor lag/drooping of the DIPJ is unlikely to cause long-term functional issues in patients. The brain adapts to the position of the finger in the medium to long term, so surgical treatment is very rare.
It is normal for the DIPJ to be stiff on coming out of the splint. This will improve with normal use of the hand.
It is normal for the patient to have tenderness, redness +/- a bump over the area of injury just proximal to the nail. This can take many months to settle down.
It would be extremely unlikely and rare for any surgery to be offered to patients for extensor lags following mallet injuries. Repair of the tendon to the bone does not tend to result in long term improvement. DIPJ fusion will straighten the joint at the expense of any bend in the joint. DIPJ fusion may be useful in cases of osteoarthritis of the DIP joint, but the pain experienced tends to be self-limiting and resolves in time.













