Information
Note:
Behaviourally induced sleep restriction, or ‘voluntary’ sleep restriction, is the commonest cause of sleepiness in our community!
This generally comes down to poor sleep habits, poor sleep hygiene, poor lifestyle and not making sleep a priority. There may be bedroom safety issues and poor sleeping environments, including bed poverty.
Average sleep requirements are 7-8 hours a night for most adults. Some may get by with less (generally not under 4 hours a night) and some may need up to 10 hours a night to function adequately.
Other causes of excessive daytime sleepiness are listed in the figure below.
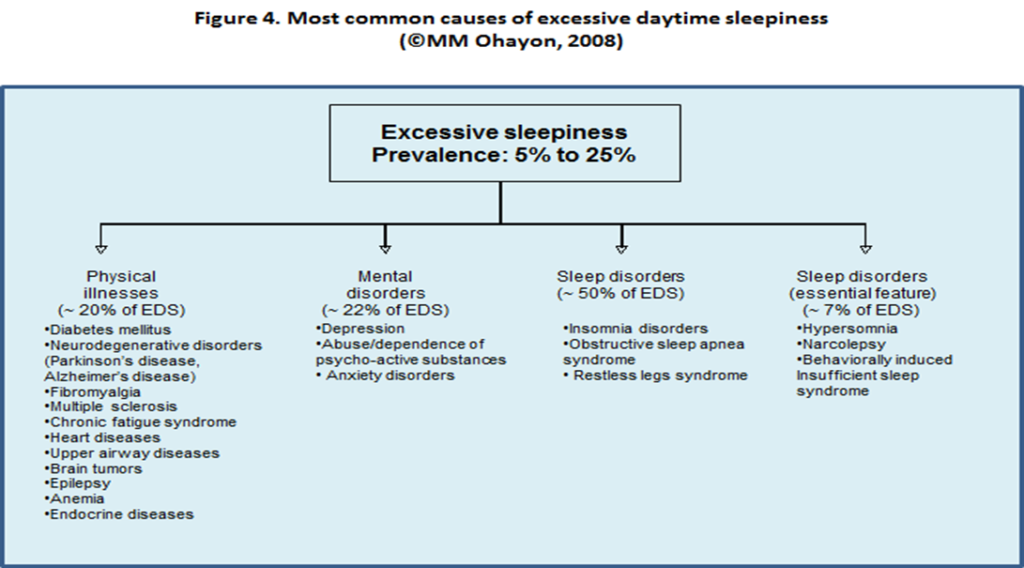
NOTE: Anxiety disorders are very frequently missed as a cause of EDS.
Diagnostic Tools
Generally, a simple history of excessive daytime sleepiness is sufficient. Clearly, physical examination and basic tests are crucial.
The Epworth Sleepiness Scale is helpful. For more information on rarer causes of excessive day time sleepiness see link
Who can refer:
Any healthcare professional
Whom to refer:
Any patient in whom a sleep disorder is thought to be contributing to or wholly causing excessive daytime sleepiness.
Essential criteria for referral
- Sleep diary of at least 4 weeks to ensure that sleep times are regular. Sleeping in at the weekend is a sign of chronic partial sleep deprivation and should be addressed first. Sleep Diary AASM
- Delayed sleep phase should be addressed fully prior to referral – this can be diagnosed on a sleep diary for at least 4 weeks see Circadian Rhythm Disorders – RefHelp
- Sleep hygiene has been addressed.
- Medications reviewed.
- Lifestyle has been addressed: exercise, caffeine, alcohol, drugs and smoking.
- Any medical and psychiatric issues fully addressed.
ALL patients must have the following undertaken and addressed, if necessary, prior to referral:
Full blood count
U’s & E’s
Liver function tests
Thyroid function tests
Full iron studies (Low Ferritin can cause fatigue and must be greater than 100mcg/l when Restless Legs Syndrome is suspected to allieviate symptoms)
Folate
B12
Vit D levels (if patient meets criteria as per ICE eg evidence of osteomalacia, malabsorption etc)
HbA1C
Chest radiograph, BBV screen and pregnancy testing as well as testing for cortisol deficiency, low testosterone and low female hormones may be useful in selected cases.
Who not to refer:
Insomnia – see Insomnia – RefHelp
Restless legs syndrome – see Restless Legs Syndrome (RLS) – RefHelp
Delayed sleep phase syndrome – see Circadian rhythm disorders – RefHelp
Behaviourally induced sleep insufficiency
Psychiatric disorders unless a primary sleep disorder is suspected.
Anyone with abuse or dependence issues that have not been addressed first.
We welcome referrals for advice only, if it is felt the patient would benefit from review in clinic this will be offered in addition
How to refer:
Sci-gateway: RIE > Respiratory Sleep > LI Sleep Referral
Or headed letter to:
Department of Sleep Medicine
Royal Infirmary of Edinburgh
51 Little France Crescent
EH16 4SA
- Appropriate treatment of the condition diagnosed: primary sleep disorder
- Treatment of the medical disorder causing sleepiness or fatigue
- Addressing disorders of sleep initiation and maintenance
- Adequate sleep! (7-8 hours, maybe more)
- Restructure daily activities to include enough time for sleep
Basic Sleep Hygiene and Questions around Sleep
- Regular sleep and waking times
- Avoid exercise right before bedtime
- Increase daytime exposure to bright light
- Caffeine, nicotine, alcohol, food, fluid intake and timing
- Environment; devices and late-night bright light
- Replacing medications that cause fatigue
- Regular exercise and moderate aerobic activity
- Recognition and discussion of stress
- Trial of antidepressants/anxiolytics for 6 weeks if anxiety or depression is suspected. Please ask the patient directly. They often deny these symptoms and have not been given time to open up about them.













