Diagnosis of New Cases of COPD
- spirometry – an assessment of severity based on % predicted FEV1
- chest x-ray
- possibility of a new alternate diagnosis
- patient responds to treatment
- patient condition is worsening
- body mass index
- MRC dyspnoea scale (see below)
- exacerbation frequency
- alpha 1 antitrypsin deficiency – should be suspected and referred to respiratory physician if the patient is:
- under 45 years old
- of Caucasian descent
- if family has a history of COPD
- record comorbidity.
| Medical Research Council (MRC) Breathlessness Scale | |||||
| Grade | 1 | 2 | 3 | 4 | 5 |
| Degree of breathless-ness related to activities | Not troubled by breathlessness except on strenuous exercise. | Short of breath when hurrying or walking up a slight hill. | Walks slower than contemporaries on level ground because of breathlessness or has to stop for breath when walking at own pace. | Stops for breath after walking about 100m or after a few minutes on level ground. | Too breathless to leave the house, or breathless when dressing or undressing. |
Differential diagnosis of COPD
Asthma
- Onset early in life (often childhood)
- Symptoms vary from day to day
- Symptoms at night/early morning
- Allergy, rhinitis, and/or eczema
- Family history of asthma
- Largely reversible airflow limitation
Bronchiectasis
- Large volumes of purulent sputum
- Commonly associated with bacterial infection
- Coarse crackles on auscultation
- CXR/CT shows bronchial wall thickening
Congestive cardiac failure
- Fine basilar crackles on auscultation
- CXR shows dilated heart, pulmonary oedema
- PFTs show restriction
Indications for hospital assessment or admission for exacerbations of COPD
- Marked increase in intensity of symptoms, such as sudden development of breathlessness at rest
- Severe underlying COPD
- Onset of new physical signs(e.g. cyanosis, peripheral oedema)
- Failure of exacerbation to respond to initial medical management
- Significant comorbidities
- Frequent exacerbations
- Impaired level of consciousness
- Confusion
- Diagnostic uncertainties
- Older age
- Insufficient home support
Who to refer:
For confirmation of new cases of COPD, consider referring for Spirometry only (which includes reversibility to salbutamol) using the ‘Primary Care Spirometry request’ form in Gateway
| Reason | Purpose |
| There is diagnostic uncertainty | Confirm diagnosis and optimise therapy |
| Suspected severe COPD | Confirm diagnosis and optimise therapy |
| Onset of cor pulmonale | Confirm diagnosis and optimise therapy |
| Frequent exacerbations (two or more/year) | Optimise therapy |
| Rapidly progressive course of disease (a rapid decline in FEV1, progressive dyspnoea, decreased exercise tolerance) | Encourage early intervention |
| Assessment for oxygen therapy | Optimise therapy and measure blood gases |
| Assessment for long-term nubuliser therapy | Optimise therapy and exclude inappropriate prescriptions |
| Assessment for oral coticosteroid therapy | Justify need for long-term treatment or supervise withdrawal |
| Bullous lung disease | Identify candidates for surgery |
| Assessment for pulmonary rehabilitation | Identify candidates for pulmonary rehabilitation |
| Assessment for lung volume reduction surgery | Identify candidates for surgery |
| Assessment for lung transplantion | Identify candidates for surgery |
| Dyfunctional breathing | Confirm diagnosis, optimise pharmacotherapy and access other therapies |
| Aged under 40 years or a family history of alpha-1-antitrypsin deficiency | Identify alpha-1 antitrypsin deficiency, consider therapy and screen family |
| Uncertain diagnosis | Make a diagnosis |
| Symptoms disproportionate to lung function deficit | Look for other explanations |
| Frequent infections | Exclude bronchiectasis |
| Haemoptysis | Exclude carcinoma of the bronchus |
Who not to refer:
- See above
- See management advice for patients with stable COPD
How to refer:
Use Sci Gateway for referral to these services.
- Royal Infirmary of Edinburgh, Respiratory Medicine Clinics, Spirometry only or respiratory OP clinic
- Western General Hospital, Edinburgh, Respiratory Medicine Clinics, Spirometry only or respiratory OP clinic
- St. Johns Hospital, Howden, Livingston, Respiratory Medicine Clinics
- Leith CTC, Respiratory Medicine Clinics, Spirometry only or respiratory OP clinic
- Click here for details about the Edinburgh Community Physiotherapy Respiratory Team
- Click here for details about Midlothian Community Respiratory Team.aspx
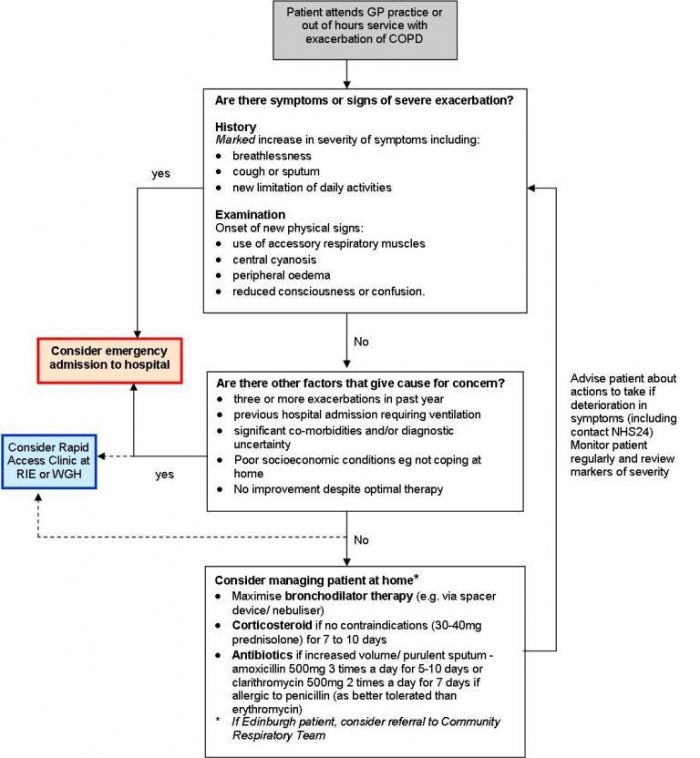
Protocol for management of COPD exacerbation in primary care
Many patients with an exacerbation of COPD can be managed successfully at home. However, there should be a low threshold for emergency admission to hospital for patients with evidence of a severe exacerbation of COPD and for those who do not respond to initial treatment. Decisions about management of a patient with an exacerbation of COPD will vary depending on the patient’s individual circumstances including the severity of their underlying disease, the presence of other medical conditions, and their social situation.
The following algorithm provides guidance for the management of COPD exacerbations in primary care (for use in GP practices and out of hours service).