Information
Pre-diabetes is characterised by the presence of blood glucose levels that are higher than normal but not yet high enough to be classed as diabetes. If undiagnosed or untreated, pre-diabetes can develop into Type 2 Diabetes (T2D).
For this reason, pre-diabetes is often described as the grey area between normal blood sugar and diabetic levels and is a risk factor for cardiovascular disease and future Type 2 Diabetes.
Diagnosing Pre-diabetes
Pre-diabetes is a state of early insulin resistance and can be diagnosed with a single HbA1c of 42-47, but it also encompasses impaired fasting glycaemia and impaired glucose tolerance.
If a pre-diabetes state is diagnosed using glucose criteria, HbA1c should be checked as a baseline and should be used for follow-up purposes. An individual with IFG and/or IGT may have an HbA1c ≤41 mmol/L at baseline, but they should still be diagnosed and coded as pre-diabetes.
Coding implications
In Lothian we recommend using the umbrella code Pre-diabetes (WITH the hyphen)*
#C11y5 Pre-diabetes
You may also wish to consider an additional recall code could such as: 66Az High risk of diabetes annual review**
However consideration may be given to frailty and whether it is in patient’s best interests to code and the frequency of appropriate monitoring.
* when performing future QI, audit or similar, we would still recommend you include R102.11 Pre-diabetes in searches for the condition to capture those coded this way historically.
** this code can be used for ALL high risk patients on one recall, includes Gestational diabetes, Long term high dose steroids (> 5mg for > 3 months), PCOS over 40Y)
These definitions are shown in Table 1 in the Resources and Links section. Note the recent change in fasting glucose threshold to align with updated SIGN guidelines 2025, fasting plasma glucose now 6.1-6.9.
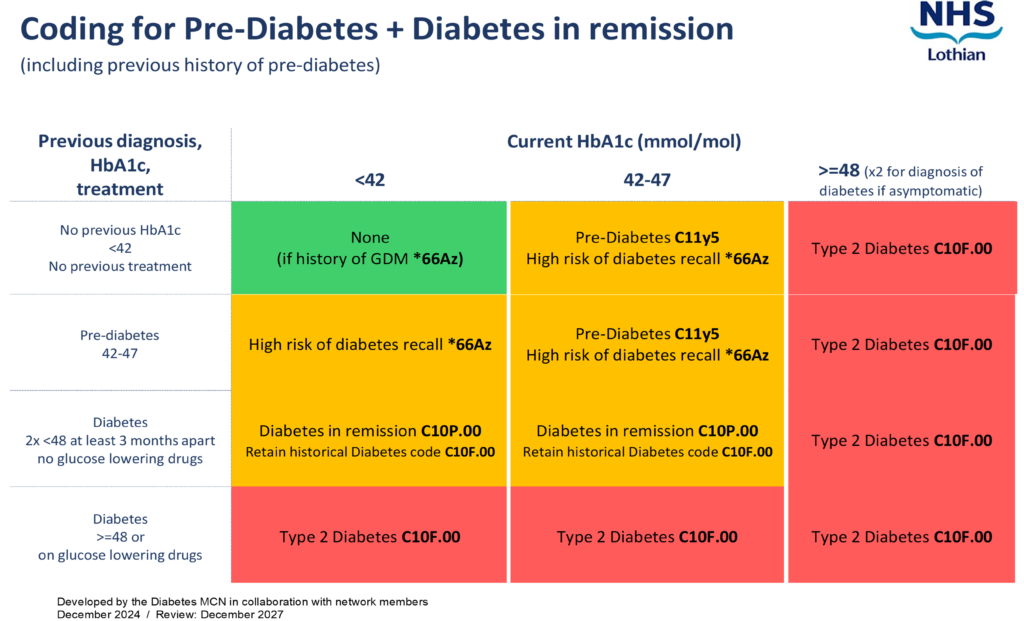
https://apps.nhslothian.scot/files/sites/2/Pre-diabetes-Dynamic-Coding-Infographic-December-2024.pdf
Let’s Prevent Diabetes Programme
Let’s Prevent Diabetes (LPD) is a structured 6-hour group education programme for those with Pre-diabetes (HbA1c 42-47), including Impaired Fasting Glycaemia and Impaired Glucose Tolerance, as well as other patients who are at high risk of developing Diabetes.
LPD educates and supports patients into developing self-management plans via trained educators from within the Lothian Weight Management and Type 2 Diabetes Prevention Team.
Patients attending Educator led sessions are offered follow up refresher appointments at 3-month intervals for 12 months, supporting long term adherence to self-management plans.
M.A /D.R.M & A.C 06-08-24
Who to refer:
Refer patients with Pre-diabetes (HBA1C 42 – 47 or impaired fasting glucose or impaired glucose tolerance) or patients who are at high risk of developing diabetes for other reasons (see under primary care management tab for advice regarding risk stratification).
Patients can be given a copy of this information leaflet about LPD: Lets Prevent Diabetes.pdf
Patients that have had previous Gestational Diabetes (GDM) are at increased risk of future T2D, so those with GDM are automatically offered LPD post-partum as part of the Lothian GDM Pathway. There may be people with a history of previous GDM some years ago, direct referrals to LPD are welcomed at any time from this cohort.
Patients with PCOS are often high risk. Consider risk stratification and testing.
Further information on programmes, links to healthy lifestyle resources and contact details can be found on the NHS Lothian Adult Weight Management and Type 2 Diabetes Service web page.
Who not to refer to LPD:
- Patients already diagnosed with T2D. The DESMOND programme and My Desmond digital health pathway is designed to provide early intervention and education for those newly diagnosed.
- Patients with only a low/moderate risk of Diabetes (See details in Primary Care Management section)
- Patients who do not have a diagnosis of prediabetes but may require weight management support.
How to refer:
AHP – Dietetics – Let’s Prevent Diabetes – LI Let’s Prevent Diabetes
Referrals are accepted from all health care professionals via sci-gateway or by letter, email or referral form to Weight Management Mailbox.
Please visit Weight Management Service Adult – RefHelp (nhslothian.scot) page for more information.
Patients are able to self refer to Let’s Prevent Diabetes programme using this form Adult Weight management Referral form.pdf
Primary care teams play a significant role in the identification of patients with pre-diabetes, those who are at High risk of diabetes and also those at moderate risk of developing diabetes.
At risk groups include those known to be at increased risk of T2D, due to the risk factors below.
Risk Factors:
- Age: Over 40 years old (white Caucasian) or over 25 years old (African-Caribbean, Black African or South Asian)
- Family history: 2-6 times more likely to develop T2D if a parent, brother, sister or child has diabetes
- Ethnicity: T2D is 2-4 times more likely in people of South Asian descent and African-Caribbean or Black African descent*
- Overweight: BMI over 25 (white Caucasian) or over 23 (African Caribbean, Black African or South Asian)
- Waist circumference:
- Women: 31.5 (80-cm) inches or over
- Men: 35 (90 cm) inches in south Asian men, 37 (94cm) inches in white or black men
- High blood pressure or previous heart attack or stroke
- Polycystic ovary syndrome
- Previous gestational diabetes*
- Severe mental health problems including those prescribed Clozapine and Olanzapine which are known to induce weight gain and increase risk of T2D.
If a patient has a number of the above, the more at risk they are of developing T2D.
Patients may wish to help and calculate their score online
1. Calculate and code RISK score:
This can be calculated via the Diabetes UK Know Your Risk Tool , which requires patients to measure height, weight and waist circumference, or the Leicester diabetes score (abbreviated form the DUK know your risk tool) which is available on Vision+
NICE guidelines encourage keeping an up to date register of RISK scores, along with introducing a recall system to invite those at risk of Type 2 Diabetes in for regular review. This is also an opportunity to support patients to manage lifestyle changes and encourage goal setting.
2. Manage RISK score:
Please note SIGN guideline recommend FPG range 6.1-6.9 in line with WHO guidelines. Any patients affected have been highlighted to their GPs by the PCCO (Feb 2025)
NICE Guidelines: Managing Risk of Type 2 Diabetes
3. Lifestyle changes
Lifestyle changes with the aim of managing excess weight and increasing exercise are pivotal to the prevention of diabetes, but consider all the pillars of health
- Dietary patterns – A Healthy Balanced Diet. There is some evidence for Mediterranean, DASH diet, whole foods plant based and low carbohydrate diets but the most important changes are ones patients are motivated to stick with. For more information about the individual programmes for weight management visit Weight Management Service Adult – RefHelp (nhslothian.scot) .
- Please ask patient about their levels of participation in Physical Activity, Recommending a slight increase to general recordation’s of trying to accrue 30 mins of Moderate Activity every day,(210mins over the week) where the patient is breathing a little deeper and working a little harder than normal, in line with recommended guidance for those with Pre and Type 2 Diabetes. If seeking additional guidance, Physical Activity support can be offered & provided by Local partners. Referral pathways into accessing these services in Lothian exist to support patients into accessing supported activity from:
- Edinburgh Leisure
- Enjoy Leisure (East Lothian)
- Excite (West Lothian)
- Midlothian Active Choices
- Healthy sleep (Better Sleep – Wellbeing Lothian)
- Stress management (Dealing with Stress – Wellbeing Lothian)
- Discuss harmful substance avoidance (alcohol/smoking)
4. Monitoring of Pre-diabetes
Pre-diabetes is monitored with an annual HbA1c, unless symptoms develop prior to this. Those that have attended LPD, making changes and attempting to impact HbA1c levels should be offered a HbA1c test 3 months post LPD completion.
Advise patients to look out for the following:
- Polyuria
- Polydipsia
- Change in eyesight
- Weight loss
- Lethargy
- Thrush oral/genital
| Normal | Pre-Diabetes | Diabetes | |
|---|---|---|---|
| HbA1c (mmol/mol) | ≤ 41 | 42-47 | ≥ 48 |
| Fasting glucose (mmol/l) | ≤ 5.4 | 6.1-6.9 | ≥ 7.0 |
| 2-hr glucose in OGTT (mmol/l) | ≤ 7.7 | 7.8-11.0 | ≥ 11.1 |
| Random glucose (mmol/l) | ≥ 11.1 |
At risk of T2D is defined as being at Moderate to High risk of T2D via the Diabetes UK Know Your Risk Tool.
High risk T2D is defined as those with previous or current Gestational Diabetes, those with Poly Cystic Ovary Syndrome or those with Prediabetes.
Online education
MyWay ealearning: Type 2 Diabetes Prevention Online Course | Information Site
Diabetes UK: Prediabetes | Diabetes UK | Reduce risk type 2 diabetes
Lets Prevent Diabetes – Adult Weight Management and Type 2 Diabetes Prevention Service
NICE Guidelines: Type 2 Diabetes: Prevention in People at High Risk
NICE Interactive Flowchart: Risk Assessment for Type 2 Diabetes
British Heart Foundation: Measuring Waist Circumference
Moving Medicine: Physical activity leaflet













