Background
Coeliac disease is common (affecting approximately 1% of the general population), but it is estimated that around two thirds of patients remain undiagnosed.
The condition is more common in those with:
- A positive family history (approx. 10% lifetime risk)
- Other autoimmune disease e.g. Type 1 Diabetes, thyroid disease (approx. 5% prevalence)
- Specific syndrome groups e.g. Down Syndrome, Turner, Williams’ (approx. 5% prevalence)
The management of coeliac disease in children & young people (<16years of age) across Lothian is Dietetic-led with Paediatric GI consultant input.
The Paediatric Coeliac Service is informed of all positive coeliac serology results directly from the WGH Biochemistry Laboratory. The dietetic team will then get in touch with you to inform you of the results and request a formal referral to the Paediatric Coeliac Service using SCI-GW. Following referral the family are contacted directly to arrange a supportive new patient consultation and discussion around diagnosis and plan further investigation and ongoing management. All patients with positive coeliac serology who are referred to the service must continue to eat adequate amounts of gluten and not to go gluten free until instructed otherwise by secondary care.
Children and young people with existing coeliac disease can also be referred to the Paediatric Coeliac Service using SCI-GW.
Where the primary care team feels additional expertise is required, an ‘advice only’ referral can be made to the Paeds GI team using SCI-GW or advice requested via the service email.
Any queries or questions relating the Paediatric Coeliac Service can be emailed to cyp.coeliac@nhslothian.scot.nhs.uk
If a diagnosis is made either ‘no-biopsy’ or following endoscopic assessment, the Dietitians will see and enrol the patient into the GFFS.
There is no need for GPs to enrol the patients into the service.
Who to test:
Both of the following ‘who to test’ guidelines are relevant
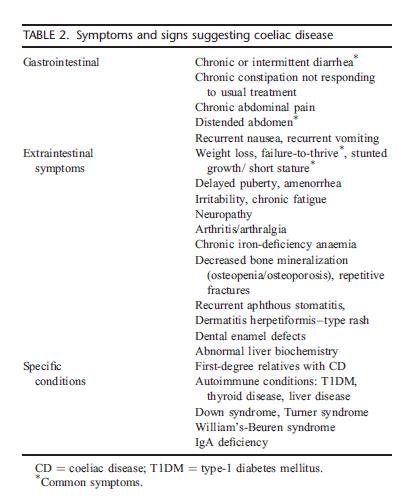
Current symptoms and signs to consider testing is in Table 2 (guidance from ESPGHAN 2020)
Coeliac disease investigation is quick and relatively easy – anti-TTG IgA serology is very reliable.
Testing should be considered and performed in anyone who:
- has associated symptoms (see the table below), or
- is in known ‘at-risk’ group (ie family member, relative), or
- is worried they may have the condition.
It is important that patients are tested whilst on gluten – if they are gluten-free, then they should be advised to restart normal diet and then be tested in 6 weeks.
If someone feels it would be difficult to do a challenge and cannot go back onto gluten they can be discussed with the coeliac service through an Advice only referral as to what options there are for testing and management.
Patients should not be referred up to the GI service to have those tests organised. This can be done by primary or secondary care either directly in practice, or where necessary via the RHCYP phlebotomy service but should there be any potential issues or problems we are very happy to discuss..
NICE NG 20 who to test:
https://www.nice.org.uk/guidance/ng20/chapter/Recommendations#recognition-of-coeliac-disease
J.B & P.G. 27-02-24
Who to refer:
All children and young people under age 16 with and positive IgA tTG antibody > 5 units/ml who are continuing to eat gluten.
Patients with selective IgA deficiency (sIgAD) and children with a low IgA who have triggered the laboratory to perform an IgG tTG test and it is positive IgG tTG (>10 units/ml).
Any existing CYP Coeliac Service patient under age 16 where there is advice required about their coeliac disease management or related issues
Any ‘Advice only’ Coeliac related question: e.g. who to test, when to test, how often etc. This may include those who may have gone gluten free and are seeking expert advice.
IMPORTANT – All patients with positive results who are referred to the service must continue to eat adequate amounts of gluten until instructed otherwise by secondary care.
How to refer / ask advice:
To Paediatric Coeliac Service using Sci-Gateway.
RHCYP>General Medicine>LI Paediatric Coeliac Services
Advice also available to all HCP via CYP.Coeliac@nhslothian.scot.nhs.uk
Lothian GFFS Gluten free information: https://services.nhslothian.scot/GlutenFreeFoodService/Pages/default.aspx
NHS Inform: https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/coeliac-disease
Coeliac UK: https://www.coeliac.org.uk/information-and-support/coeliac-disease/about-coeliac-disease/
https://www.coeliac.org.uk/information-and-support/living-gluten-free/kids-teens-and-young-adults/
NICE NG20: https://www.nice.org.uk/guidance/ng20













