Primary care clinician within NHS Lothian – Lumbar spine pathway | Right Decisions
MSK Physiotherapy for people with lumbar spine problems is provided as part of the NHS Lothian Integrated Back Pain Pathway.
The NHS Lothian integrated back pain pathway is a multidisciplinary collaboration. The service is based on the principles of the right care, from the right person, at the right time in the right place. The service offers a single point of access for patients with routine low back pain and lumbar spine related leg symptoms pain who require referral for their problem following failure to improve with initial primary care management.
Once within the service patients will be able to access all the multidisciplinary services that are required for their problem including physiotherapy, investigation, surgical opinion and pain clinic opinion. There will be no need for patients to return to their GP to seek additional referrals or investigations for the lumbar spine problem. The service is underpinned by agreed pathways, escalation criteria and multidisciplinary clinics.
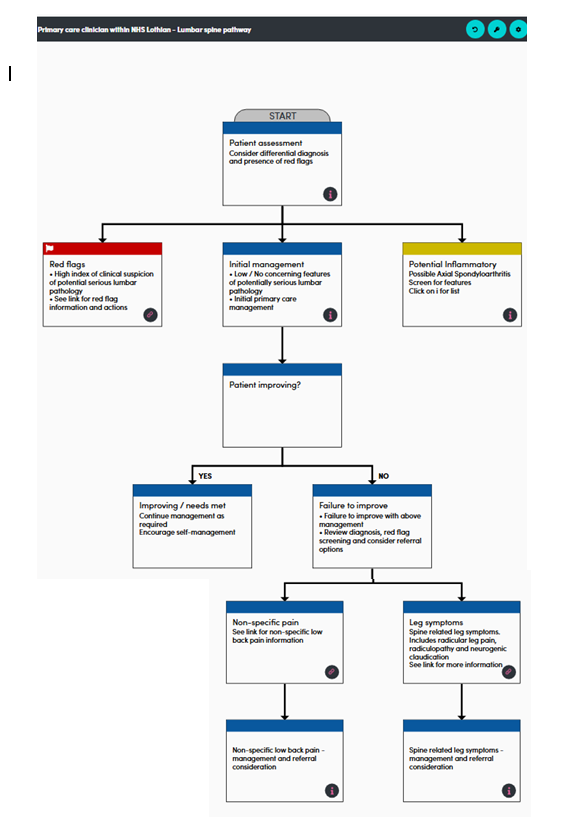
- For clinical support, referral guidance and interactive flowchart above, see Spine pathways | Right Decisions (scot.nhs.uk)
- For patients & professionals – NHS Lothian Integrated Back Pain Pathways & service homepage
M.A & P.A. 12-03-25
Who can refer:
- All primary care clinicians i.e. GPs, Primary care MSK advanced practice physiotherapists, advanced nurse practitioners
- Patient self referral (resident of East Lothian HSCP, Edinburgh HSCP and West Lothian HSCP Where To Find Us – Musculoskeletal Physiotherapy)
- Secondary care consultants and associated teams
- MSK physiotherapists are able to escalate/refer to spinal advanced practice physiotherapists underpinned by agreed pathways and processes NHS Lothian Integrated Spinal Service
Who to refer:
- All routine cases of low back pain and spine related leg symptoms who have not responded to initial primary care management within a 4-6 week period and do not have the presence of significant red flags nor have suspected inflammatory spinal pain – see sections serious lumbar spine conditions and other considerations and inflammatory spinal pain
- Spine related leg symptoms- Consider earlier referral in cases intractable symptoms and/ or developing motor deficit but without significant red flags and suspected neurogenic claudication in which symptoms are beginning to affect quality of life and the ability of the patient to look after themselves.
- Non-specific low back pain in the absence of a dominant psychological component who have not received recent physiotherapy for their condition or who have received physiotherapy previously for their condition but;
- have experienced a substantial change in their presentation
- require assistance with achieving a functional goal
- wish further assessment and considerations of management options
- have clinical features suggestive of an underlying specific cause for their lower back pain i.e. spondylolisthesis, spondylolysis, in which further investigation would guide management (other than serious spinal pathology).For further support & guidance and refer to: Spine pathways | Right Decisions (scot.nhs.uk)
- MRI scan is not required at point of referral. If a MRI is indicated as part of a patients management this will be requested within the multi-disciplinary service at the appropriate time for the patient and any intervention that may be required. A patient leaflet to support this decision has been created in conjunction with Neurosurgery, Neurology, Radiology, GPs and Physiotherapy within NHS Lothian available below.
Who not to refer:
- Patients who have the presence of significant red flags/ suspicion of serious lumbar spine condition or have suspected inflammatory spinal pain – see Serious lumbar spine conditions (Red Flags) – RefHelp
- Age <16
- Chronic back pain with a significant psychological / psychiatric / drug addiction element/ pain causing significant distress & disability, no planned referral to another speciality for diagnosis or treatment of pain – see Chronic pain Chronic Pain – RefHelp.
How to refer:
- For all cases of routine low back pain / spine related leg pain – refer via SCI Gateway Referral “AHP-Physiotherapy” then choose local site.
- This single referral will gain access to the full multidisciplinary NHS Lothian integrated back pain pathway. Any subsequent investigation/ surgical opinion/ pain service referral will be made within the service
- Please include all relevant details on your referral to allow the appropriate initial triage of the patient. Initial triage will occur within MSK Physiotherapy and if appropriate will be passed to spinal advanced practice physiotherapy service.
- Please signpost patients to Integrated Spinal Service Webpage for patient information.
Other information
For all routine cases of low back pain and spine related leg pain who meet the criteria under “who to refer”, referral to other specialities including Orthopaedics, Neurosurgery, Neurology & Rheumatology is not indicated. Once within the service patients will be able to access all the multidisciplinary services that are required for their problem including physiotherapy, investigation, surgical opinion and pain clinic opinion. There will be no need for patients to return to their GP to seek additional referrals or investigations for the lumbar spine problem. The service is underpinned by agreed pathways, escalation criteria and multidisciplinary clinics.
Non specific low back pain and spine related leg symptoms – For further information see associated sections
Key information
- Provide advice on information and support – for example: NHS Lothian MSK Self-help information webpage
- Offer reassurance and advice on self-management strategies
- Provide information and advice on the natural history of back pain & spine related leg symptoms to encourage realistic expectations.
- Reassure that acute non-specific low back pain is unlikely to have a serious structural cause, and most people recover within weeks.
- Sciatica symptoms usually settle within a few weeks to a few months, but in some people they may persist for longer and recurrence is common.
- Encourage the person to keep active, resume normal activities, and return to work/study as soon as possible.
- Discourage prolonged bed rest. Reassure that normal back movements may produce some pain, but this is not harmful if activities are resumed gradually. Advise there is no need to be pain-free before resuming normal activities.
- Consider the short-term application of local heat (such as a heat pack).
- Advise to keep as active as possible and exercise regularly to reduce the risk of recurrent episodes.
- Optimise medication, if needed – see NICE Guideline NG59 for specific recommendations
- Provide information on when they should seek follow up and when to seek immediate medical attention
- Consider advising the person to arrange review if symptoms persist or are worsening, timescales will vary depending on clinical judgement.
- Advise the person to seek urgent medical review if there are red flag symptoms or signs suggesting a potentially serious underlying cause.
Patient leaflet: Integrated Low Back Pain Service PIL
Patient leaflet: For further guidance and Low-Back-Pain-and-MRI-scans.pdf
For guidance and support refer to Spine pathways | Right Decisions (scot.nhs.uk)
Vertebral-Fragility-Fractures-Pathway-V21.pdf
Scottish Referral Guidelines for Suspected Cancer (Malignant Spinal Cord Compression):
https://www.cancerreferral.scot.nhs.uk/malignant-spinal-cord-compression/
NHS Lothian patient website https://services.nhslothian.scot/IBPS/Pages/default.aspx
Integrated Low Back Pain Service PIL














