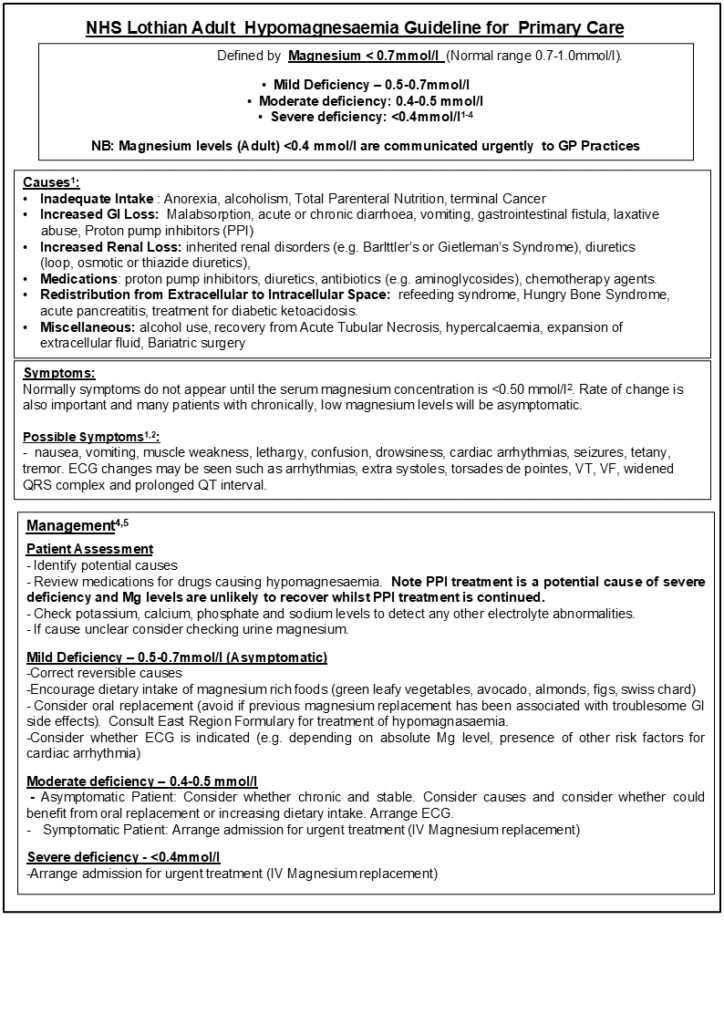
GPs are not expected to screen for, or monitor, magnesium levels and this guidance is intended to help in the uncommon situation where GPs are contacted about a low magnesium result.
Hypomagnesaemia is generally diagnosed in two ways in the primary care setting:
- Where there is a VERY LOW CALCIUM (eg <1.9) where the labs will ‘reflexly’ test for hypomagnesaemia which is probably driving this. The likely outcome would be admission for intravenous calcium and magnesium. This is a very rare event and most commonly associated with long-term PPI use.
- Sporadic cases – often diagnosed during an inpatient stay, relating to acute illness and outlined in the guidance below.
Symptoms of low serum magnesium are non-specific, but the more severe cases are associated with conditions often needing hospital admission.
CM & SJ 25.09.25
1. Ayuk J, Gittoes NJ. Contemporary view of the clinical relevance of magnesium homeostasis. Ann Clin Biochem. 2014 Mar;51(Pt 2):179-88. doi: 10.1177/0004563213517628. Epub 2014 Jan 8. PMID: 24402002.
2. ZS. Agus. Hypomagnesaemia. J.Am. Soc. Nephrol. 1999, 10:1616-1622.
3. The communication of critical and unexpected pathology results (Royal College of Pathologists, 2017) Microsoft Word – Comm Crit Results Final version.docx (rcpath.org)
4. BMJ Best Practice Assessment in Magnesium Deficiency (Updated 16 July2024)Assessment of magnesium deficiency – Differential diagnosis of symptoms | BMJ Best Practice
5. East Region Formulary (Formulary | East Region Formulary (nhs.scot))
6. Hypomagnesia – a guideline for GPs https://www.ruh.nhs.uk/pathology/documents/clinical_guidelines/PATH021_Hypomagnesaemia_Guideline.pdf













