Services
| Clinic | Specialist advice contact details |
| Lipid Clinic, RIE | RIE.LipidClinicAdvice@luht.scot.nhs.uk |
| Lipid clinic, SJH | Tel: 01506 523 841 |
| Lothian lipid guidelines | Lothian Lipid Guidelines.pdf |
Lothian Hypertriglyceridaemia Guidelines (Confirmed May 2019).pdf
Seek specialist advice:
- If TG >10
- TG 5–10 in a high cardiovascular risk patient not responding to statin treatment
- Suspected familial hyperlipidaemia
- Patients with significant hyperlipidaemia that is proving difficult to manage in primary care
- Refer urgently to secondary care those with TG >20 not caused by alcohol or poor glycaemic control
Triglycerides (TG) (mmol/L)
- Routinely measured as part of a full lipid profile to enable LDL calculation.
- TG testing in isolation is rarely indicated.
- Can be elevated on a non-fasting sample due to the presence of dietary TG, consider fasting sample.
- Very high TG levels e.g. >10mmol/L are associated with pancreatitis; increased morbidity and mortality independent of CVD risk.
- High TG are most commonly due to secondary causes e.g. poorly controlled diabetes mellitus, alcohol excess or medications.
- The relationship between TG and cardiovascular risk is unclear. Overall it is felt that raised TG still confer a small degree of additional risk.
Clinical assessment
- Examine for any skin changes suggestive of a primary hyperlipidaemia
- Check TFTs, fasting blood glucose (click here for more information on the diagnostic work-up for diabetes), renal function, liver function, MCV and GGT
- † Consider any relevant secondary causes e.g. review medications
- Further tests as appropriate e.g. pregnancy test, urinalysis to check for proteinuria
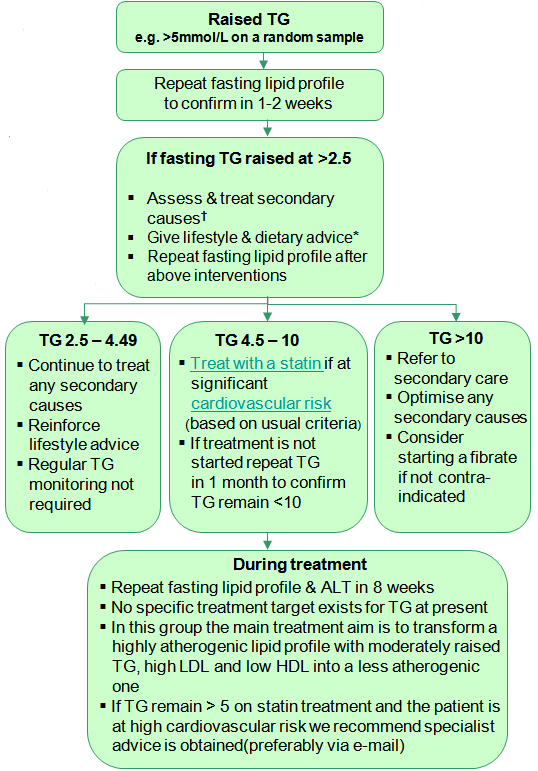
- Treat with a statinif at significant (based on usual criteria)
† Secondary causes of raised TG
- Alcohol excess
- Hypothyroidism
- Nephrotic syndrome/ renal disease
- Immunoglobulin excessDrugs (including thiazides, non-cardioselective beta blockers, oestrogens, tamoxifen, corticosteroids)
- Bulimia
- Pregnancy
- Obesity
- Insulin resistance
- Diabetes
- Metabolic syndrome
* Lifestyle advice
- Weight loss, if appropriate
- Reduce or abstain from alcohol
- Dietary modification:
reduce total calorie intake by minimizing intake of fats and carbohydrate
increase intake of fish, especially oily fish - Smoking cessation (smoking independently increases TG levels)
- Increase physical activity
More information is available at the University of Edinburgh site Home blood pressure monitoring | Lothian Hypertension and Lipid clinics & Measuring blood pressure | Lothian Hypertension and Lipid clinics













