The EXPPECT Pelvic Pain and Endometriosis Services (www.exppectedinburgh.co.uk) are tertiary multidisciplinary services primarily based at the Royal Infirmary of Edinburgh that only see referrals from secondary care. The EXPPECT pelvic pain service encompasses gynaecology, pain medicine, pain psychology, physiotherapy and acupuncture (and a pelvic pain management programme) – hence separate referrals to these specialties are not required. The EXPPECT endometriosis service encompasses gynaecology, pain medicine, pain psychology and physiotherapy, colorectal surgery and urology (with input from cardiothoracic surgery and respiratory medicine). Both services are supported by a dedicated specialist nurse.
University of Edinburgh centre-reproductive-health EXPPECT Pelvic Pain Info for Clinicians
Referral Pathway for women presenting with chronic pelvic pain in the community
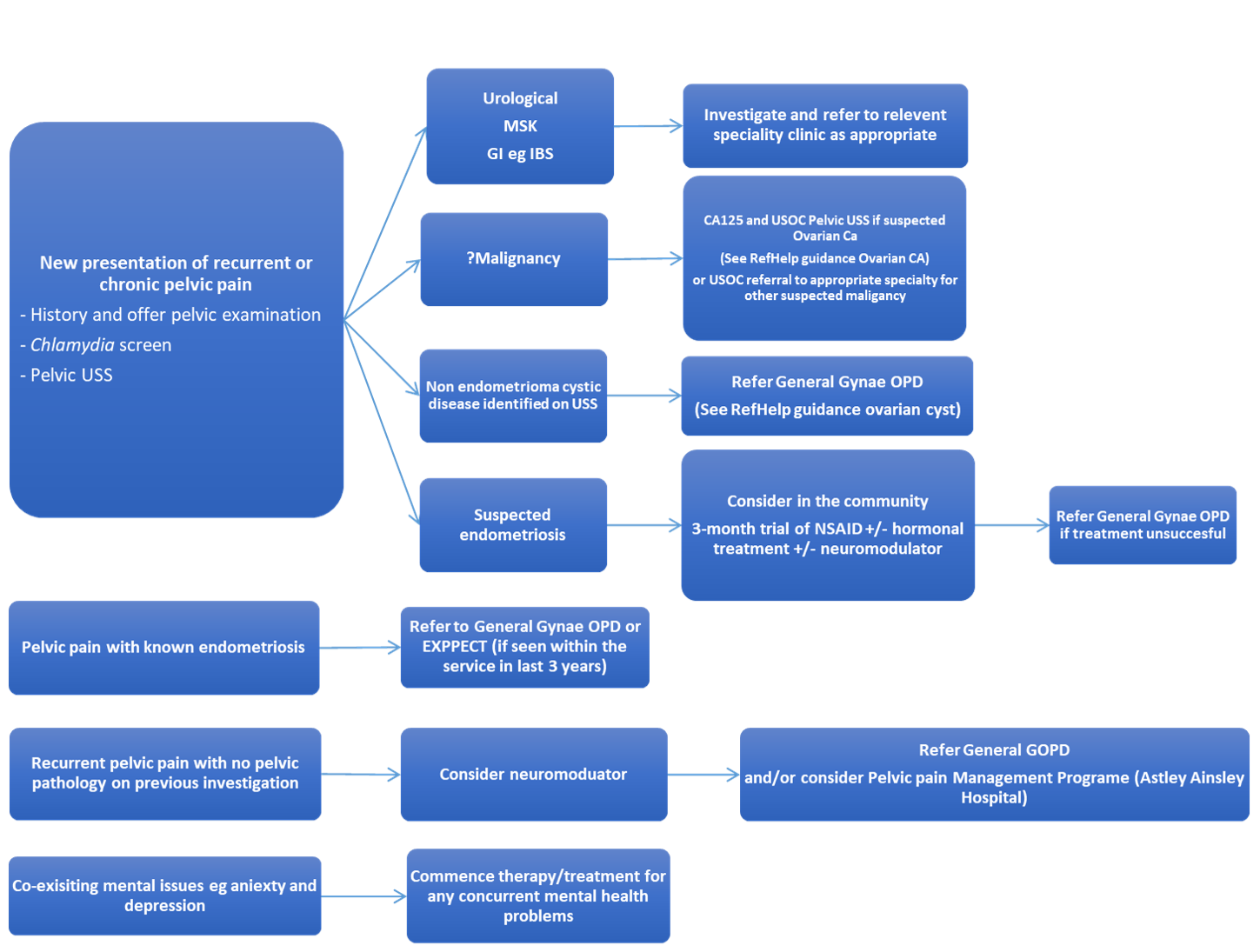
All new GP referrals for pelvic pain and suspected endometriosis should be referred directly to general gynaecology (and not to the EXPPECT service).
Who can refer to the EXPPECT Pelvic Pain and Endometriosis Services?
NHS Consultant Gynaecologists and Pain Management Consultants only (unless patient has been seen within the service within the last three years in which case mark the referral for EXPPECT).
Who can refer to the Pelvic Pain Management Programme (Astley Ainslie Hospital)?
General practitioners (please use referral pathway for Chronic Pain Management Programme).
How to refer:
For endometriosis or pelvic pain requiring secondary care assessment please refer via Sci-gateway General Gynaecology
If a patient presents with dyspareunia as a primary symptom (without pelvic pain), please refer directly to community physiotherapy
When investigating a patient with chronic pelvic pain it is important to consider gynaecological and non-gynaecological causes. It is important to note that some 40%-55% of women with chronic pelvic pain in secondary care appear to have no obvious underlying pathology based on clinical history, examination, and investigations.
Common gynaecological conditions associated with chronic pelvic pain include;
- Endometriosis
- Adenomyosis
- Chronic pelvic inflammatory disease
- Adhesions
Common non gynaecological causes include;
- Irritable Bowel Syndrome – see RefHelp guidance on diagnosis and management of IBS
- Bladder Pain Syndromee.g. interstitial cystitis
- Nerve entrapment
- MSK pain
Symptoms suggestive of endometriosis include;
- Chronic pelvic pain
- Period-related pain (dysmenorrhoea) affecting daily activities and quality of life
- Deep pain during or after sexual intercourse
- Period-related or cyclical gastrointestinal symptoms, in particular, painful bowel movements
- Period-related or cyclical urinary symptoms, in particular, blood in the urine or pain passing urine
- Infertility in association with 1 or more of the above.
Investigations for endometriosis
All patients should have the following investigations for suspected endometriosis
- Gynaecological history including smear history and consider pelvic examination
- Chlamydia screen
- Trans vaginal pelvic USS
For suspected ovarian ca please organise usoc pelvic uss and ca125
Management of endometriosis includes
- 3 month trial paracetamol +/- NSAID
- Hormonal therapy including; OCP, progestogens & Mirena IUS all equally as effective for pain relief but different side effect profiles.
- Neuromodulators
Neuromodulators for chronic pelvic pain (with no pathology identified) or Endometriosis
Amitriptyline 10mg increased every 2 weeks to 50mg or alternative tricyclic (Imipramine or Nortriptyline)
Gabapentin 300mg increasing by 300mg each week to a maximum 2700mg (in 3 divided doses)
It is not uncommon to see depression and anxiety in those suffering from chronic pelvic pain. Please consider screening for this in primary care during a chronic pelvic pain consultation and treat as appropriate. There is a computerised CBT programme in NHS Lothian for people with chronic pain with mild to moderate anxiety and depression.
https://www.nice.org.uk/guidance/ng73
https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_41.pdf
Self-management strategies to consider to combat endometriosis symptoms during the COVID-19 pandemic
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7263080/pdf/hoaa028.pdf













