Background
Secondary amenorrhoea is defined as absence of menses for 3-6 months in those with previously regular menses, or 6-12 months in those with previous oligomenorrhoea. It occurs in 3-5% of women of reproductive age, with polycystic ovary syndrome (PCOS) being the most common cause.
Secondary amenorrhoea can be physiological in nature, e.g. pregnancy, lactation.
In those with no signs of androgen excess (e.g. hirsuitism, acne, virilisation), secondary amenorrhoea can be caused by dysfunction of any aspect of the hypothalamic-pituitary-ovarian axis including:
- Hypothalamic dysfunction, secondary to:
- Pituitary dysfunction, secondary to:
- Premature ovarian insufficiency (POI)
Other causes include
- Uterine pathology
- Hypo- or hyperthyroidism
- Iatrogenic causes (e.g. medication causing high prolactin levels, delay in return of menses post-contraception)
If signs of androgen excess are present, then the causes of secondary amenorrhoea include:
- Polycystic ovary syndrome (PCOS)
- Cushing’s syndrome
- Late onset congenital adrenal hyperplasia
- Androgen secreting tumours
Secondary amenorrhoea can have long term health effects, both physical and psychological. If it is associated with low oestrogen levels, then the patient is at risk of osteoporosis and cardiovascular disease. If it is associated with anovulation, then infertility can be an issue and patients can be at increased risk of endometrial pathology, such as endometrial hyperplasia.
Who to refer:
Patients with:
- Blood results consistent with premature ovarian insufficiency
- Blood results consistent with hypogonadotrophic hypogonadism
- Certain patients with PCOS (see specific PCOS RefHelp guidance – link below)
Poly Cystic Ovary Syndrome – RefHelp (scot.nhs.uk) - Patients with hyperprolactinaemia
- Patients with increased testosterone levels (>4nmol/L)
- Recent history which could indicate possibility of Asherman’s syndrome or cervical stenosis (e.g. recent surgical evacuation of the uterus, cervical surgery, severe pelvic infection)
- Lack of menses for >12 months in context of normal bloods
Who not to refer:
Those with primary amenorrhoea and <16 years old should be referred to the Paediatric Endocrinology team.
It may be more appropriate to refer some patients to the General Endocrinology team, including patients with:
- Hyperthyroidism
- Features of Cushing’s syndrome or late-onset congenital adrenal hyperplasia
If the patient is actively trying to conceive, then referral to the Infertility Clinic may be more appropriate.
Management within Primary Care is appropriate in those with:
- Menopause if women 40 years old and over
- Hypothyroidism
How to refer:
Refer via SCI-Gateway – RIE – Gynaecology – Reproductive Endocrine
1. Exclude pregnancy, lactation and menopause.
2. History: menstrual, sexual, contraceptive, medical, psychiatric (including eating disorders), drug, diet, recent weight change, stress, exercise.
3. Examination:
- BMI
- Features of excess androgen (acne, hirsuitism, virilisation)
- Visual field assessment (if suspicious of pituitary tumour)
- Features of thyroid disease
- Features of Cushing’s syndrome
- A PV exam may be appropriate
4. If the patient’s LMP was less than 6 months ago:
- Reassure
- Treat other medical conditions as necessary
- Reassess at 6 months
If the patient’s LMP was 6 or more months ago, perform the following investigations in Primary Care:
- Blood tests: FBC, FSH, LH, oestradiol, prolactin, TFTs, testosterone, sex hormone binding globulin (SHBG) and free androgen index (FAI)
Interpretation of Blood Results
| HypogonadotrophicHypogonadism | PCOS | POI | Hyperprolactinaemia | |
| FSH | Low/normal | Normal | High | Normal/low |
| LH | Low | Normal/slightly high | High | Lower than FSH |
| Oestradiol | Low | Normal | Low | Low/normal |
| Prolactin | Normal | Normal/slightly high | Normal | High |
| Testosterone | Normal | Normal/slightly high | Normal | Normal |
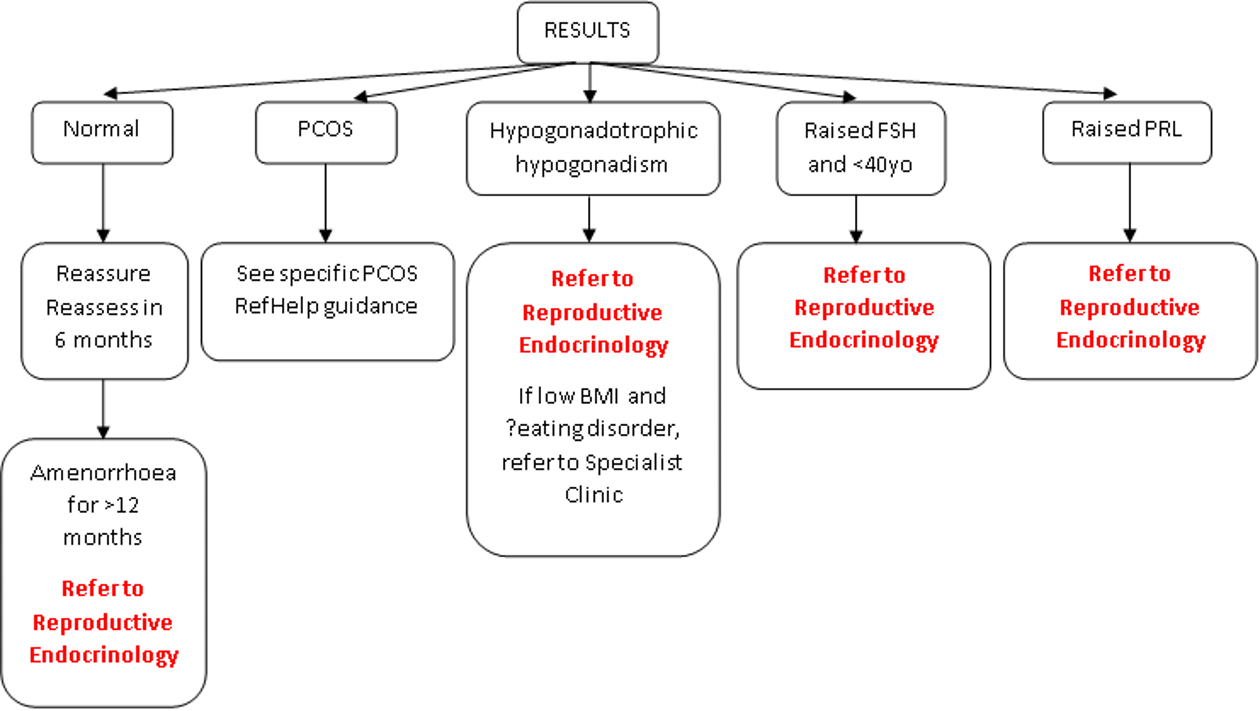
Action on Blood Results – see action pathway below
- Pelvic ultrasound: if diagnosis is unclear from blood results
5. Provide psychological support as required
6. If amenorrhoea lasts more than 12 months and is associated with low oestrogen levels, then consider whether osteoporosis prophylaxis is required (e.g. dietary and lifestyle advice, HRT if appropriate, annual review with DEXA scans every 3-5 years)
NICE Clinical Knowledge Summary – https://cks.nice.org.uk/topics/amenorrhoea/













