There is helpful, patient-friendly information and advice to be found on the GI section of the NHS Lothian Internet pages. There are also some videos by our very own GI team which patients have been responding very positively to. Consider sharing the link with patients and/or carers.
If seeking referral then please make sure the IBS Diagnostic Pathway has been followed, including exclusion of red flags and up to date blood tests and bowel tests have been done. This pathway has been created to ensure that there are appropriate safety filters in terms of history and diagnosis, to ensure that red flag diagnoses are not missed, and to ensure that the referral is not returned to primary care because of missing investigations.
Background:
- Irritable bowel syndrome (IBS) affects 10-20% of the adult population
- Females are twice as likely to present as males
- Symptoms are most common in those ages 20-30
Consider a POSITIVE diagnosis of IBS in patients with any of the following symptoms for >6 months:
- Abdominal pain related to defaecation
AND
Two of:
- Related to defecation
- Change in stool frequency
- Change in stool form
Features such as bloating, lethargy, nausea, backache and bladder symptoms are common in people with IBS and may be used to support the diagnosis.
IBS Diagnostic Pathway
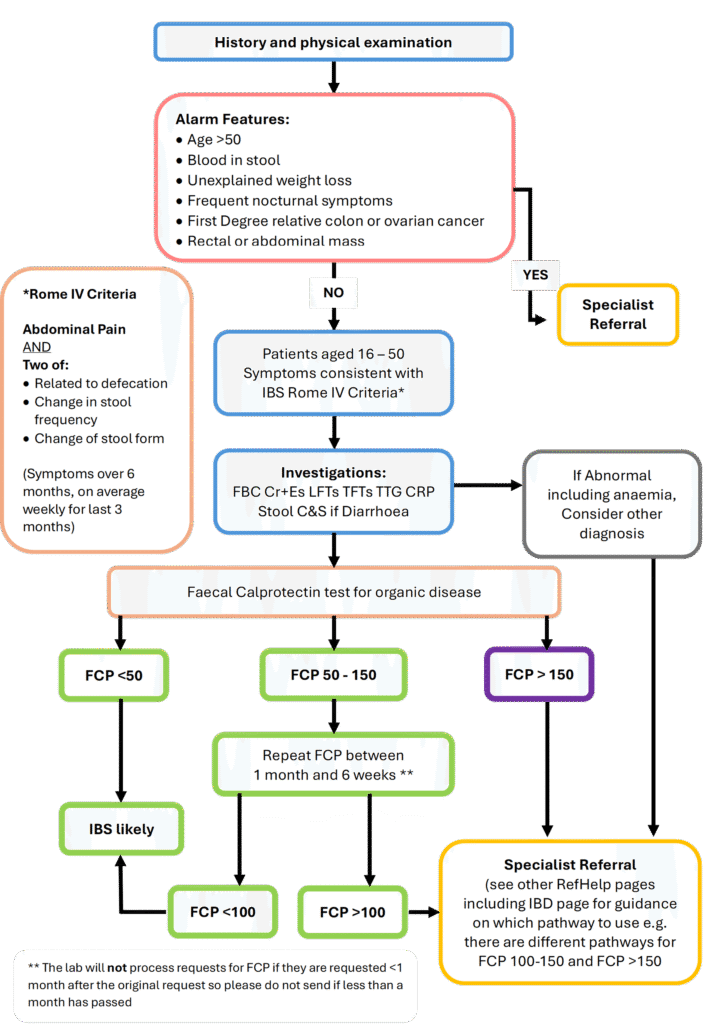
This is the current IBS Diagnostic Pathway. There are currently national discussions on an overall Lower GI the pathway, and changes will be made to RefHelp once a national pathway has been agreed and adopted locally.
NOTES.
- Family history of colon cancer is especially relevant if a first degree relative (FDR) <50yrs is affected, or if there are 2 FDRs affected at an older age. Clinical Genetics have comprehensive guidance on FH of Colorectal Cancer.
- Faecal calprotectin is useful in identifying patients with a higher probability of organic colonic disease
- In patients with persistent watery diarrhoea not responding to Rx, consider the possibility of microscopic colitis and possible need for colonic biopsies.
- If you are considering a diagnosis of IBS due to symptoms including Chronic Diarrhoea, please remember that unexplained chronic diarrhoea is an HIV indicator condition and HIV testing should be considered.
IBS Post Diagnostic Information for Patients
There is helpful, patient-friendly information and advice to be found on the GI section of the NHS Lothian Internet pages. Consider sharing the link with patients and/or carers.
The text to share for a link (can copy and paste) is: https://services.nhslothian.scot/GI/IBS/. Alternatively, if the patient is in the room with you and has a smart phone with them, you can bring up the page, right click and choose create QR code for this page and the patient will then have a link to the page on their phone.
These videos below have been created by GI and they are all patient directed videos. Please share them with patients as you feel appropriate.
IBS Post Diagnostic Management and Referral Pathway
This is a pathway for LOW RISK patients with a DEFINITE DIAGNOSIS of IBS who are suitable for Dietetic led support. For this reason the pathway is only suitable for those aged under 50 years of age. Those patients who are 50 or over, even if they were diagnosed when they were younger, should be referred to the Gastroenterology team.
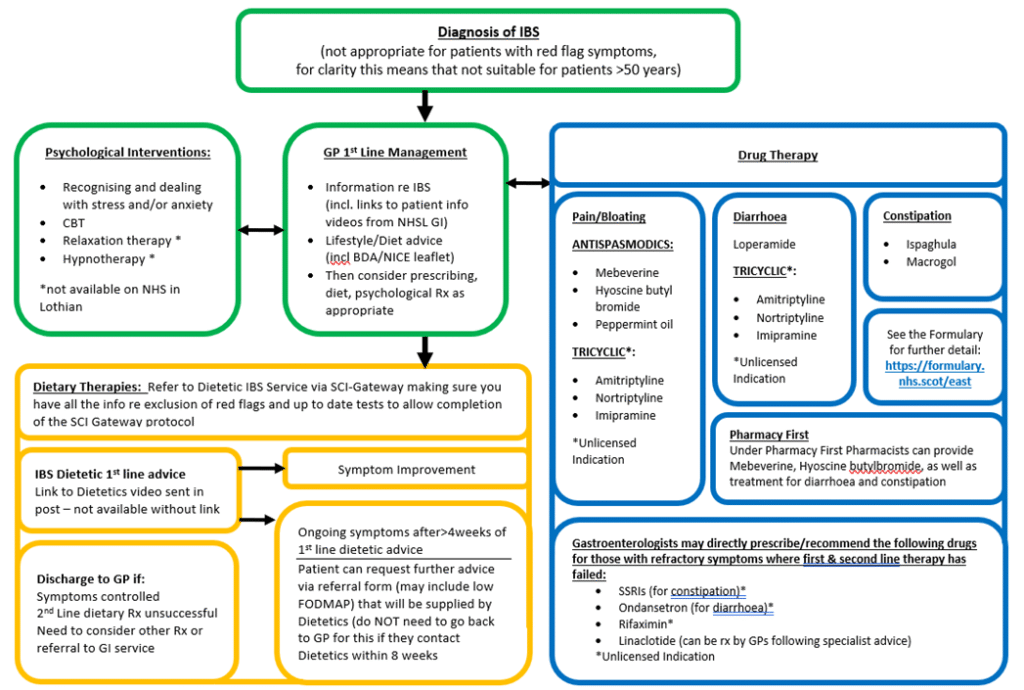
Please see further guidance on management of IBS in Primary Care under the Primary Care Management tab below.
Please remember that a low FODMAP diet is not suitable for everyone. Please do not issue low FODMAP information as this advice should be supported by a FODMAP trained dietician.
Please see pathway above for how referral fits into the IBS-Post Diagnostic Management and Referral Pathway.
Referral is to Dietetics IBS Service via SCI Gateway using the following pathway:
AHP – Dietetics >> Adult IBS >> LI Adult IBS
Please be aware that there is protocol text that must be completed for the referral to be accepted. The protocol text requested includes requiring an affirmative response to all of the following:
- Confirmation that the patient does not have any alarm features (see above for details)
- Recent (at least within the past 5 years) Faecal Calprotectin result for patients
- Recent Coeliac serology
- Recent FBC Cr&E, LFT, TFT, CRP
- Stool C&S if patient has a history of diarrhoea
- Confirmation that the patient meets the Rome IV criteria for the diagnosis of IBS and a positive diagnosis has been made
The protocol also asks:
- If the patient is pregnant
As well as information on the main page re medication and patient resources, the following information may also be helpful:
General Points
- Irritable Bowel Syndrome is NOT a diagnosis of exclusion
- It can be diagnosed POSITIVELY using simple clinical criteria and ruling out certain red flag symptoms and other conditions by simple tests available in Primary Care (see separate IBS Overview)
- Once a POSITIVE diagnosis has been made, treatment consists of reassurance and symptom relief.
- This requires a very good understanding of what the symptoms are so a good history is vital
- Different approaches to treatment work better for different individuals and it is often necessary to trial a number of different approaches
- A failure of one or two therapies is frustrating but common. It is not, in itself an indication that the primary diagnosis is wrong.
Outline of therapy
- Selection of diet, drug or psychological interventions will be influenced by patient preference and local availability. Combination approaches may be appropriate for some patients.
- Drug therapies “below the line” should currently be regarded as primarily for specialist initiation.
Dietary Advice
- If written information is to be given to your patient, we would recommend this first line advice sheet: Nice BDA IBS advice leaflet
- Approximately 50% of IBS patients will achieve some level of symptom relief after implementing these guidelines
- Re low FODMAP Diet: Please do not issue low FODMAP information. A low FODMAP diet is not suitable for everyone
- A low FODMAP diet has proven effective in 70-75% patients when supported by a FODMAP-trained dietician
- A low FODMAP diet can be very restrictive and may exclude certain foods which are beneficial to long-term gut health. It should only be followed with dietetic support for a short period of time before the reintroduction process is initiated
Specific Management Guidance
These are links to PDFs that are for clinicians managing patients who have IBS:
NICE & BDA IBS advice leaflet (PDF)
NICE Irritable Bowel Syndrome guidance (website)
Please also see under Primary Care Management for a selection of NHS Lothian produced patient information leaflets













