People with inflammatory bowel disease (IBD) may be seen in WGH, RIE and St John’s. The IBD nurse helpline and biologics service for Edinburgh are based in WGH. SJH also provide a biologics service and IBD nurse helpline for patients in West Lothian.
When referrals are made via the IBD SCI GW Referral Pathway for a possible new diagnosis of IBD we aim to:
- Provide rapid clinic access/diagnostic tests (with dedicated IBD colonoscopy slots)
- Provide rapid treatment of newly diagnosed IBD
- Ensure continuity of treatment for people on biologic or other IBD therapies moving into the area
- Provide ongoing care for those patients with an established IBD diagnosis made outwith NHS Lothian and who now require follow up in NHS Lothian
Please do not use the SCI gateway referral process for acutely unwell people needing urgent assessment – there is an on-call service for GI in both WGH and RIE to provide urgent real time advice and admission if necessary. Please see the Referral Guidelines section for further information about referral for admission vs. OP referral.
In addition to the SCI Gateway referral process for new patients we also offer:
- IBD Consultant advice via email (usual response time within 48 hours) loth.wghibdconsultants@nhs.scot
- IBD Nurse helpline for patient advice:
WGH: 0131 537 1272
SJH: 01506 523861
- Specialty specific website for patients and NHS staff with further information on IBD
https://services.nhslothian.scot/GI/IBD
This site also includes a copy of the IBD flare card and the RCP CCUK IBD tool kit, as well links to information on the shared care agreements for azathioprine, methotrexate and mercaptopurine
J.B. & E.W. 16-05-25
Who can refer:
A competent clinical decision maker e.g. GP ST, GP ANP, GP
Who to refer:
SUSPECTED NEW DIAGNOSIS OF IBD, well enough currently for OP investigation
- Diarrhoea is the most common symptom, but this is not present in all. Other symptoms can include bloody diarrhoea, nocturnal defecation bowel urgency, high stool frequency, weight loss, abdominal pain or cramping, bloating, lethargy, fevers, night sweats, and anaemia. Constipation can occur in some patients.
- The symptoms can overlap with many other lower gastrointestinal conditions, including bowel cancer, coeliac disease, endometriosis and ovarian cancer, and IBD can occur in patients with a previous diagnosis of Irritable Bowel Syndrome (IBS).
- Consider IBD in patients with unexplained fever, weight loss, anaemia, a family history of IBD or extra-intestinal manifestations (EIM) such as arthritis, erythema nodosum, pyoderma gangrenosum, primary sclerosing cholangitis, uveitis, iritis or episcleritis.
- These symptoms should prompt further investigation as per the algorithm below, which uses testing for Faecal Calprotectin to help differentiate between IBD and IBS.
SUSPECTED NEW DIAGNOSIS OF IBD: when and how to use Faecal Calprotectin testing
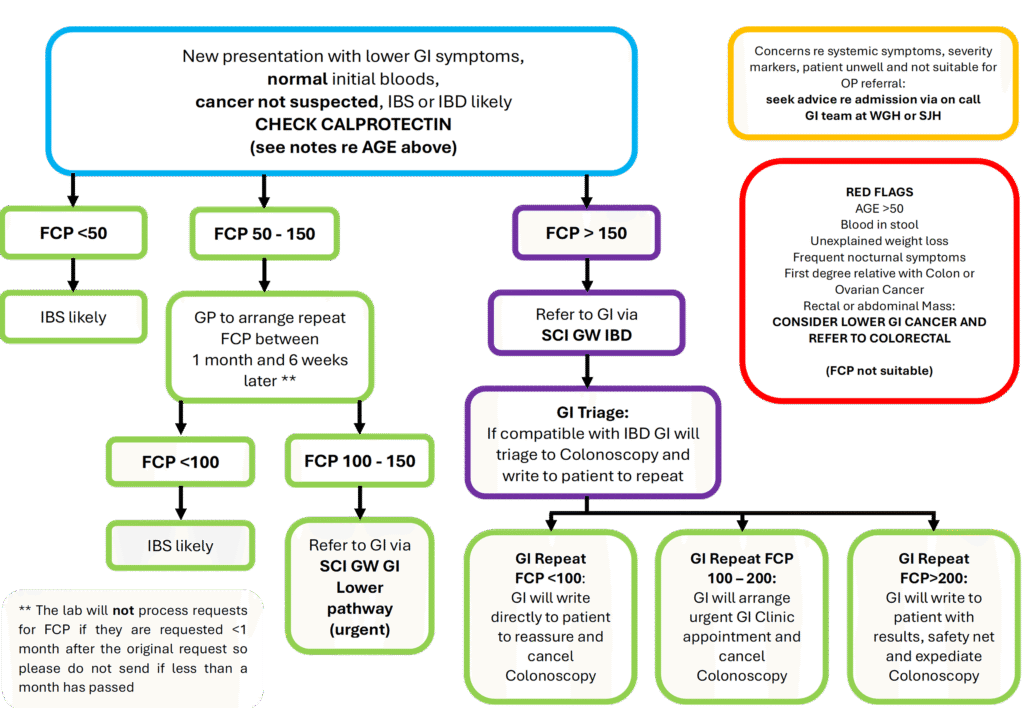
- This algorithm covers the use of Faecal Calprotectin to help differentiate between IBD and IBS in whom cancer is not suspected.
- This algorithm should be used for those with normal bloods. Anaemia, high CRP etc are abnormalities that mean referral should be considered even without high FCP. Patients with normal bloods, but high FCP may have IBD, and this is where FCP is very useful to differentiate between IBD and IBS in younger people.
- Age is important – calprotectin is used in Lothian for patients under 50 with new lower GI symptoms but anyone over 40 where cancer is suspected should be referred as per the Colorectal Cancer page
- Please bear in mind that calprotectin is not a specific test for IBD, and levels will go up in other situations including infective diarrhoea, diverticulitis, and for people on certain medications including NSAIDs and PPIs. Ideally stop NSAIDs and PPIs 2 weeks prior to testing.
ESTABLISHED DIAGNOSIS OF IBD MADE ELSEWHERE
- Individuals with a pre-existing diagnosis of IBD from outwith Lothian who require follow up in Lothian can be referred via the dedicated SCI Gateway IBD pathway. Please highlight if they are on any secondary care treatment (i.e. biologics or advanced therapies etc) and if available, scan clinic or transfer letters into the referral. An up-to-date set of bloods and calprotectin would be helpful depending on symptoms and clinical condition.
Who not to refer:
- Patients with suspected lower GI malignancy – please use separate pathway: see Colorectal Cancer RefHelp page for guidance
- Patients meeting diagnostic criteria for IBS – please see guidance on RefHelp IBS page
- Patients with symptoms for less than 2 weeks – consider infective diarrhoea
- Rectal bleeding in isolation, without diarrhoea/increased stool frequency – please refer to Colorectal team.
Acutely unwell patients requiring inpatient assessment should be referred in after discussing with the on-call team NOT by SCI Gateway – see further info below.
Please do not refer patients already known to a gastroenterologist in Lothian via the dedicated SCI Gateway IBD referral pathway. Advice about these people is available via the IBD consultant email service and the individual clinician via email. Patients are also able to get in touch directly via the IBD nurse helpline in WGH (01315371272) and St John’s (01506 523861).
How to refer:
For patients with a possible new diagnosis of IBD who are suitable to wait for outpatient assessment or patients with an established diagnosis of IBD who are new to NHS Lothian please refer via SCI Gateway. Referral can be to WGH or to SJH depending on the patient’s location. The SCI Gateway referral pathway is as follows:
- WESTERN GENERAL HOSPITAL >> GASTROENTEROLOGY – MEDICAL >> LI Inflammatory Bowel Disease
OR
- ST JOHN’S HOSPITAL >> GASTROENTEROLOGY – MEDICAL >> LI Inflammatory Bowel Disease
The following tests should be taken in Primary Care prior to referral (they are required for the SCI GW protocol where referrers have to indicate if the individual tests are NORMAL or ABNORMAL (drop down menu):
- Blood tests: FBC, Cr+Es, LFTs, Ca / Alb, CRP, B12 & Folate, Ferritin, Coeliac testing
- Stool testing: FCP, C&s including parasitology
- If you are considering a diagnosis of IBD due to symptoms including Chronic Diarrhoea and/or Weight loss, please remember that unexplained chronic diarrhoea is an HIV indicator condition and HIV testing should be considered.
Who to refer urgently for consideration of admission (via GI on-call)
CRITERIA TO ADMIT PATIENTS WITHOUT A KNOWN DIAGNOSIS OF IBD
In an unwell patient with acute abdominal pain or significant bloody diarrhoea (usually over 2 weeks) and possible IBD, please consider same day referral to the gastroenterology registrar in WGH via switchboard.
Signs of toxicity include ≥ 6 bloody stools per day and one or more of following:
- temp over 37.8°C;
- CRP greater than 30 mg/L;
- Hb less than 108 g/L;
- pulse greater than 90 bpm.
If toxicity present or clinical concern contact the on-call Gastroenterologist registrar and/or admit through flow centre.
If there is peritonism (significant tenderness on abdominal examination) same day referral to the surgical team is more appropriate.
WHEN TO CONSIDER ADMISSION FOR PATIENTS WITH KNOWN UC
Symptoms of ulcerative colitis are dependent upon severity of disease and include bloody diarrhoea, rectal bleeding, tenesmus, urgency, faecal incontinence, and nocturnal defaecation.
Acute Severe UC – please consider admission via Flow Centre/GI reg on call in WGH
6 or more bowel movements/24h plus 2 or more features of systemic upset;
- visible blood in stool
- T >37.8
- HR>90
- anaemia (Hb<105)
- ESR >30 or CRP >30.
WHEN TO CONSIDER ADMISSION FOR PATIENTS WITH KNOWN CROHN’S DISEASE
Reasons for admission in people with an existing diagnosis of Crohn’s include
- Perianal sepsis/abscess (for examination under anaesthetic, usually under the colorectal team). A good rule of thumb is to refer for admission if unable to sit down properly.
- Obstruction (i.e. vomiting and post prandial abdominal pain, weight loss)
- Active Crohn’s symptoms plus systemic upset e.g. fever, tachycardia, hypotension or anaemia
After referral:
- Referrals are triaged several times a week, typically by the On Call Gastroenterology Consultant in WGH. In SJH GI team triage is also by Consultant Gastroenterologist regular
- Referrals may lead to several outcomes: Clinic appointment OR direct to test colonoscopy OR invitation to repeat calprotectin and/or qFIT (invitation from GI to patient, not via Primary Care). The triaging consultant will contact the patient directly to action these results.
- Regardless of the hospital referred to patients may be contacted to offer an appointment at a different site. If there are specific reasons that a patient would not be suitable for this, please make sure this information is included in the referral.
- It is helpful if at the time of referral, the referrer informs the patient that they may be offered an appointment at a different site.
The following tests should be taken in Primary Care prior to referral (they are required for the SCI GW protocol where referrers have to indicate if the individual tests are NORMAL or ABNORMAL (drop down menu):
- Blood tests: FBC, Cr+Es, LFTs, Ca / Alb, CRP, B12 & Folate, Ferritin, Coeliac testing
- Stool testing: FCP, C&s including parasitology
Crohn’s Disease Flare Pathway – Developed by Crohn’s and Colitis UK with RCGP
Crohn’s Flare Pathway – link to website PNG
UC Flare Pathway – Developed by Crohn’s and Colitis UK with RCGP
UC Flare pathway – link to website PNG
https://apps.nhslothian.scot/files/sites/2/NHS-Lothian-GI-UC_flare_management_pathway_June_2018_Final-2.pdf (text easier to navigate on some devices)
NHS Lothian Resources
GI-Crohns_flare_management_pathway_June_2018_FINAL.pdf (nhslothian.scot)
https://apps.nhslothian.scot/files/sites/2/GI-UC_flare_management_pathway_June_2018_Final-1.pdf
Links to flare pathways are under Primary Care Management













