Overt untreated hypothyroidism is associated with foetal loss, gestational hypertension, placental abruption, low birthweight babies, poor perinatal outcome and severe neurodevelopmental delay. The developing foetal brain requires optimal thyroxine levels from early in the first trimester of pregnancy, before foetal production of thyroid hormones begins at 12 weeks gestation. Therefore in pregnancy there is an increased requirement for T4. [1,2,3]
The offspring of women whose free thyroxine levels are in the lowest 10% of the reference range in the first trimester of pregnancy have been shown to be at risk of significant neurodevelopmental delay at the age of two years. [4] Most cases have already been diagnosed prenatally and will be on replacement therapy. If replacement is adequate, outcomes are usually very good. The commonest causes of hypothyroidism in pregnancy are Hashimoto’s thyroiditis and treated Graves’ disease.
The increase in serum free thyroxine (FT4) levels in women early in normal pregnancy does not occur in women who are hypothyroid. It is thus vital to ensure adequate thyroxine replacement from as early as 5 weeks gestation. [5]
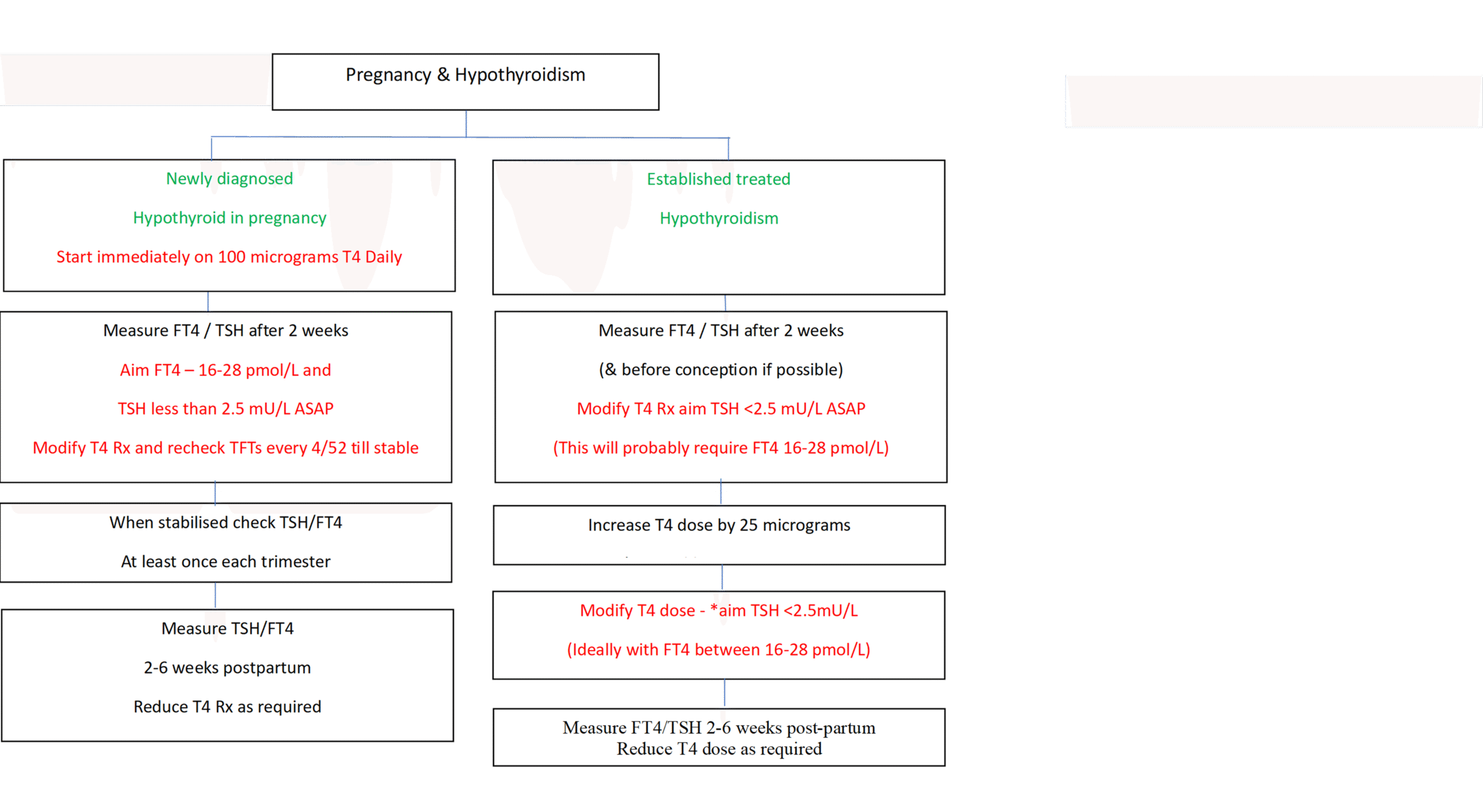
It is recommended that patients with established hypothyroidism should have the T4 dose increased by 25 micrograms when a pregnancy is confirmed.
The recommended treatment of maternal hypothyroidism is administration of oral LT4. Other thyroid preparations such as T3 or desiccated thyroid should not be used in pregnancy as the foetal CNS is relatively impermeable to T3.
Assessing Hypothyroidism in Pregnancy
Ideally women with hypothyroidism should be reviewed by their GP pre-pregnancy to ensure that they are euthyroid. All women with a history of hypothyroidism should be discussed with/referred to a consultant obstetrician. They should also be encouraged to present as soon as they become pregnant in order that their thyroxine dose may be increased and TSH and FT4 monitored regularly. Ideally, TSH should be maintained below 2.5mU/l.
For patients with established hypothyroidism the ideal monitoring regimen is therefore: –
- TFTs before conception (if possible)
- TFTs at diagnosis of pregnancy or at antenatal booking – but do not wait for these results before increasing the levothyroxine dose by 25micrograms as soon as the pregnancy is confirmed
- TFTs 2 weeks after the dose of T4 has been increased
- TFTs at least once in each trimester
- TFTs 2-6 weeks postpartum
- Women with adequately treated hypothyroidism do not require serial growth scans during pregnancy
- If hypothyroidism has been poorly controlled, the obstetrician will consider foetal growth assessment in the third trimester.
Patients with a history of Graves’ disease who are euthyroid or hypothyroid through radioiodine treatment or surgery must have TSH-receptor antibodies (TRAbs) measured early in pregnancy irrespective of the thyroid function test profile. Women are advised not to conceive within 6 months of radio-iodine therapy.
- If TRAbs are undetectable they do not need to be repeated.
- If TRAbs are positive, the patient will need to be seen by a consultant endocrinologist and consultant obstetrician. It is likely that further measurements of TRAbs will be required in these patients during pregnancy. Patients should be advised to deliver in hospital and the neonatal team must be informed at delivery. Additional ultrasound scans may be required and TSH/FT4/Total T3 on cord blood may be required (see ‘Managing Hyperthyroidism’ section below).
Patients newly diagnosed with hypothyroidism whilst pregnant should have T4 treatment commenced immediately with a starting dose of 100 microgram daily. A further assessment of thyroid function tests should be performed after 2 weeks to ensure FT4 is ideally 16-28 pmol/L; TSH should be less than 2.5 mU/L, but not suppressed. Further changes in T4 dose, followed by repeat thyroid function tests may be required to achieve this ‘ideal’ biochemical profile (16-28) – please note the ideal is narrower than the laboratory reference ranges. The aim is to replace levothyroxine as generously as possible to ensure that TSH is <2.5mU/l without suppressing TSH below the lower end of the reference range. If attempts to push the FT4 level to 16-28 pmol/L result in a suppressed TSH, a lower FT4 level is acceptable.
- As a minimum, patients should have thyroid function tests performed once each trimester
- If TFTs are unstable refer to a consultant obstetrician / consultant endocrinologist by email / SCI Gateway as early as possible as growth scans may be required.
- Women with stable, satisfactory thyroid function tests do not need to see an obstetrician but email discussion of TFTs should be initiated by community midwife. An obstetrician will see anyone about whom there are concerns.
- GPs should reduce T4 dose to pre-pregnancy dose at 2-6 weeks post-partum and recheck TSH/Free T4 6-8 weeks later.
HYPOTHYROIDISM AND PREGNANCY: KEY SAFETY POINTS
- Assess thyroid status: Preferably prior to conception or at booking in the following situations
- Known hypothyroidism
- Type 1, Type 2 diabetes
- Previous history of thyroid disorder
- Family history of thyroid disease
- Features of thyroid disease
- Other autoimmune thyroid disorder
- Hypothyroid patients should be offered an appointment with a consultant obstetrician.
- Patients with established hypothyroidism should have T4 dose increased by 25 micrograms as soon as a pregnancy test is positive.
The aim is to replace levothyroxine as generously as possible to ensure that TSH is <2.5mU/l without suppressing TSH below the lower end of the reference range. Further monitoring after 2 weeks and possible further changes in T4 dose may be required to achieve TSH <2.5 mU/L as quickly as possible. This will probably require the FT4 level to be in the ballpark of 16-28 pmol/L. However, if this results in a suppressed TSH, a lower FT4 level is acceptable.
- Measure TRAbs in all patients with a history of Graves’ disease (irrespective of thyroid status)
Patients with detectable TRAbs require special management: inform Endocrinologist/Obstetrician as soon as possible.
- Further checks on thyroid function test should be made at least once each trimester
- If TFTs are not stable contact consultant obstetrician, as a growth scan may be required.
- Hypothyroid patients should be offered an appointment with consultant obstetrician
- Cut back T4 dose to pre-pregnancy dose 2-6 weeks post-partum
PREGNANCY AND HYPOTHYROIDISM (newly diagnosed and established).
REFERENCES – please see the Resources and Links section of the main Thyroid Conditions and Pregnancy page.
C.M. & N.Z. 08-07-24













