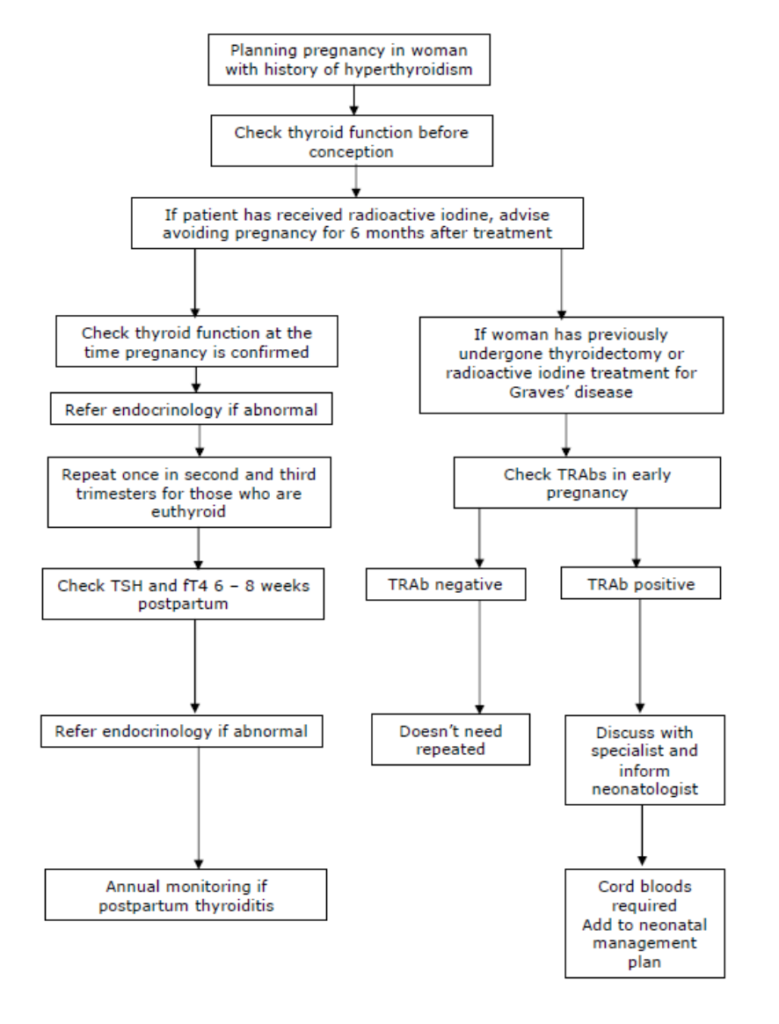
Planning pregnancy in Hyperthyroidism
TFTs and Hyperthyroidism in Pregnancy – TRAb is crucial
Patients being treated with anti-thyroid drugs require careful monitoring during pregnancy as these drugs cross the placenta and interact with the foetal thyroid. Similarly, TSH receptor antibodies (TRAbs) in maternal blood also cross the placenta and may give rise to intrauterine and neonatal thyrotoxicosis if present in high concentration.
For these reasons it is essential to identify new cases of Graves’ disease in pregnancy and also to assess TRAb status in patients with previous Graves’ Disease who may be hypothyroid or euthyroid due to therapy with radioiodine, surgery or anti-thyroid drugs.
hCG shares a common subunit with TSH and therefore has thyrotropic activity. TSH is therefore often suppressed in early pregnancy and up to 60% pregnancies complicated by hyperemesis are associated with a biochemical picture of hyperthyroidism. Urgent admission should be arranged if a woman has symptoms and signs of severe hyperthyroidism or intractable vomiting.
Significance of an ‘undetectable’ TSH in pregnancy
Some ‘normal’ pregnancies are associated with a mild transient ‘physiological’ hyperthyroidism during the first trimester. This is caused by very high levels of hCG, which has a mild stimulatory effect on the thyroid. In approximately 3% of pregnancies the TSH will be suppressed to <0.01mU/L and FT4/FT3 may be slightly elevated. It is essential to exclude Graves’ disease in such pregnancies; TRAbs should be measured, and an endocrine and/or obstetric opinion sought.
HYPERTHYROIDISM AND PREGNANCY – KEY SAFETY POINTS:
- Women with biochemical thyrotoxicosis must have TRAbs measured to exclude Graves’ disease.
- Measure TRAbs in all patients with Graves disease at booking (irrespective of thyroid status). Patients with detectable TRAbs require special management, irrespective of their thyroid function test profile: inform the endocrinologist and obstetrician as soon as possible. If TRAbs are undetectable, they do not need to be repeated.
- ALL PATIENTS WITH HYPERTHROIDISM IN PREGNANCY SHOULD BEEN SEEN BY A CONSULTANT ENDOCRINOLOGIST OR OBSTETRICIAN FROM EARLY IN PREGNANCY.
- ALL THOSE WITH A PAST HISTORY OF HYPERTYROIDISM, WHO ARE NOW EUTHYROID, SHOULD BE DISCUSSED WITH A SPECIALIST
- All women with a past or current history of hyperthyroidism who are planning pregnancy should have thyroid function checked before conception and be referred for specialist advice.
- Please see the flow diagram below.
Patients with detectable TRAbs:
- The Endocrinologist and Obstetrician should be informed of any patient with detectable TRAbs.
- Women with detectable TRAb should be advised to deliver in hospital.
- Further TRAb measurements and ultrasound scans will be required, the frequency of which will be advised by the endocrinologist and obstetrician. Typically, a scan is required each trimester, in addition to growth scans at 28 and 34 weeks (more often if control is poor).
- Paediatricians should be informed of delivery within the first 12 hours of life and the consultant obstetrician will document this in the neonatal management plan during the antenatal period. The infant should be seen within the first 24 hours of life if TRAb are detectable at 36 weeks or if the TFTs from cord blood are abnormal
- Cord blood should be taken for TSH, FT4 and Total T3 at delivery and the baby should have a resting heart rate checked and remain in hospital for at least 24 hours. Further repeat TSH, Free T4 and total T3 in the neonate should be carried out on the advice of the neonatal team.
PLEASE ALSO NOTE:
- All women with hyperthyroidism will have serial growth scans
- The aim is for good control of hyperthyroidism on the minimum dose of carbimazole (CBZ) / propylthiouracil (PTU) possible
- Home and Birthing Centre deliveries are not appropriate for women with Hyperthyroidism
Hyperthyroidism in pregnancy flowchart
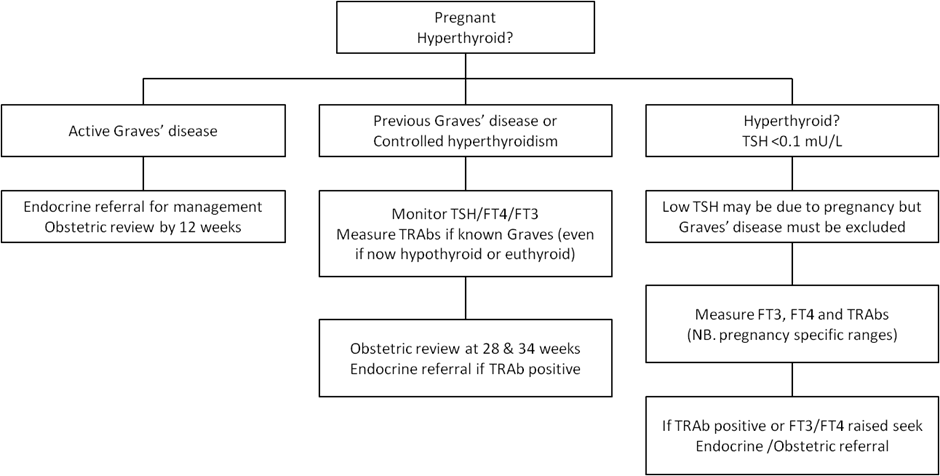
Specialist Management of Hyperthyroidism in Pregnancy
- Home delivery is not appropriate for women with hyperthyroidism, nor delivery in the Lothian Birthing Centre as the neonatal team review is required in the first 24 hours of life.
- All women with a past history of hyperthyroidism who are now euthyroid should be discussed with referred to an obstetrician. All women with hyperthyroidism will have serial growth scans.
- All women with a past or current history of hyperthyroidism who are planning pregnancy should have thyroid function checked before conception and be referred for specialist advice
- The aim is for good control of hyperthyroidism on the minimum dose of carbimazole (CBZ) / propylthiouracil (PTU) possible. For those with good control of thyrotoxicosis on doses of CBZ<15mg/day or PTU<150mg/day, the maternal and foetal outcome is usually good. The American Thyroid Association recommends use of PTU in the first trimester (to reduce the risk of congenital anomalies) with consideration being given to conversion to CBZ in the second and third trimesters (to reduce the risk of maternal liver dysfunction) [9].
Any patient with active Graves’ Disease must have TSH-receptor antibody (TRAbs) measurement carried out at first visit to community midwife (or pre-conception) irrespective of their thyroid function test profile. If TRAbs are undetectable, they do not need to be repeated.
CBZ/PTU therapy: Post Natal Management
- The endocrinologist will document a plan for the postnatal period as some women will not require CBZ/PTU treatment postnatally. However, all patients should be seen in the endocrine clinic 8-12 weeks post-partum (or sooner if symptomatic).
- Vigilance for signs of postnatal thyroid storm is essential.
- CBZ is safe in breast feeding in doses at or below 15mg daily and PTU at or below 150 mg daily.
REFERENCES – please see the Resources and Links section of the main Thyroid Conditions and Pregnancy page.
C.M. & N.Z. 08-07-24













