Fissure in ano is an extremely common and painful condition typified by a split in the anal canal associated with extreme pain on defecation and bright red rectal bleeding.
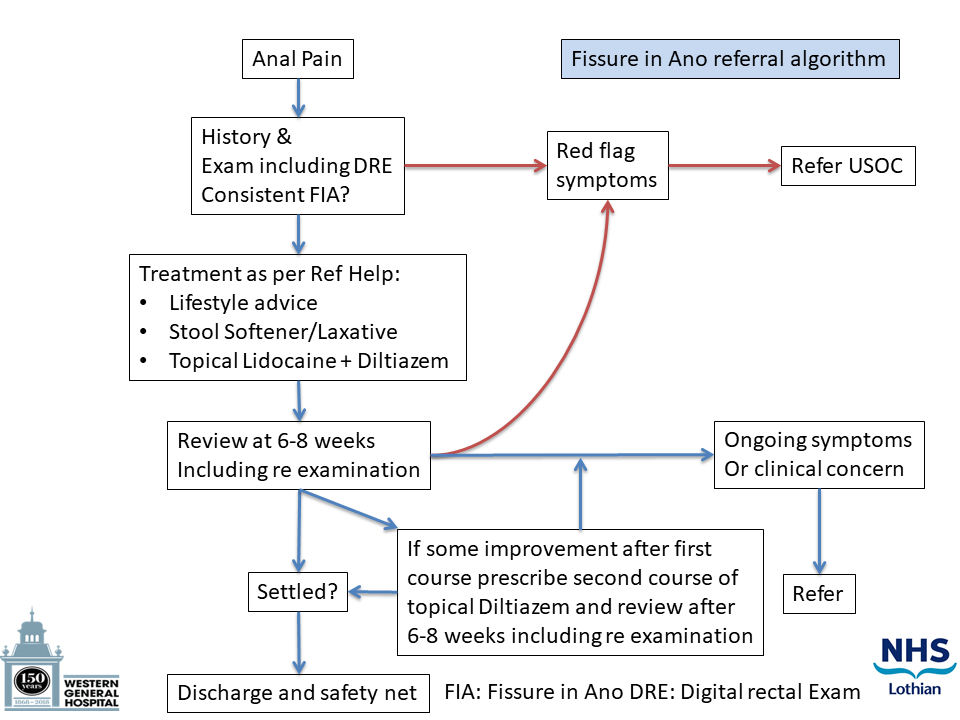
Who to refer:
Patients who are resistant to the treatments outlined in the Primary Care Management Section.
Patients in whom there is doubt about diagnosis:
- no anal fissure seen on examination. However, if their symptoms are typical of an anal fissure then it is still worth treating them, as per Primary Care Management, as well as making a referral.
- atypical symptoms
- does not fit usual patient demographic for anal fissure.
How to refer:
Via Sci Gateway to Colorectal Surgeons stating “Fissure in Ano” as the problem.
Thorough assessment
- History consistent with anal pain on defecation with bright red rectal bleeding.
- Exclude red flag symptoms and other pathologies such as Crohns, perianal warts, anal or rectal malignancy etc.
- Have a high index of suspicion in older patients presenting with symptoms for the first time.
- Perform a PR examination to visualise anal fissure(s). Patients should have a digital rectal examination to exclude any other cause of their symptoms. This could be done after a trial of treatment if the patient is too sore to be examined initially.
Approximately 80% of patients can be treated successfully using the following conservative measures.
Self-help measures to advise patients
Aim to pass stools of a soft, “toothpaste-like” consistency.
Increase daily intake of fibre. Avoid dehydration. Aim for at least 1.5-2 litres’ of fluids per day.
Get more exercise.
Don’t put off going to the toilet until later. Avoid straining to pass a stool. Avoid sitting on the toilet for too long and limit the time to 5 minutes.
Review of medications with GP or Pharmacist to check if any are causing constipation. Avoid opioid analgesics.
Keep the area clean but avoid wiping too hard. Moistened toilet tissue can be helpful but avoid wipes containing alcohol. Warm salt/sitz baths help clean the area but can also be soothing and relieve the pain.
Medications
Rationale for treatment is to soften the stool and relax the sphincter muscle. Treatment may not be successful unless both are done in conjunction.
Stool Softeners
Stool softeners can be helpful when lifestyle management methods with diet and fluids is insufficient. Avoid bulk-forming laxatives. Please see LJF for advice on prescribing laxatives.
Painkillers
Simple analgesics such as Paracetamol or Ibuprofen may help.
Topical anaesthetics (Lidocaine 5% gel) can be used before opening bowels if it is particularly painful and applied 20-30 minutes beforehand.
Relax the sphincter – Chemical Sphincterotomy
Diltiazem Hydrochloride 2% cream
If the anal fissure does not heal with the above measures then topical Diltiazem Hydrochloride can be used. It works by relaxing the anal sphincter and thereby increasing the blood supply to the fissure. This helps to aid healing of the fissure.
How it is used
A small (pea sized) amount should be applied to the finger and placed at the entrance to the anus. The cream should be used twice a day every day (morning and evening) for 2 months. It is important to complete the full course to offer the best chance of successful healing.
Prescribe 2 tubes of the cream (2 x 30gm) because this should last approximately 2 months. Review the patient after this. A second course of Diltiazem can be prescribed if the anal fissure has not completely healed after the first.
Diltiazem is usually well tolerated but potential side effects include headaches, dizziness and itchiness or burning at the site when you use the cream. Most side effects will pass within a few days.
The LJF Formulary Committee agreed in November 2020 that Diltiazem 2% cream can be “routinely available in line with local guidance”. It can be prescribed by GPs in Primary Care following the advice set out above.
The Scottish Medicines Consortium (SMC) does not recommend Glyceryl trinitrate rectal ointment (Rectogesic) for use within NHS Scotland for the relief of pain associated with chronic anal fissure.













