COVID-19:
Covid-19 prompted the British Society of Haematology to issue pandemic B12 guidance , and this outlines some of the principles for moving to oral B12 preparations.
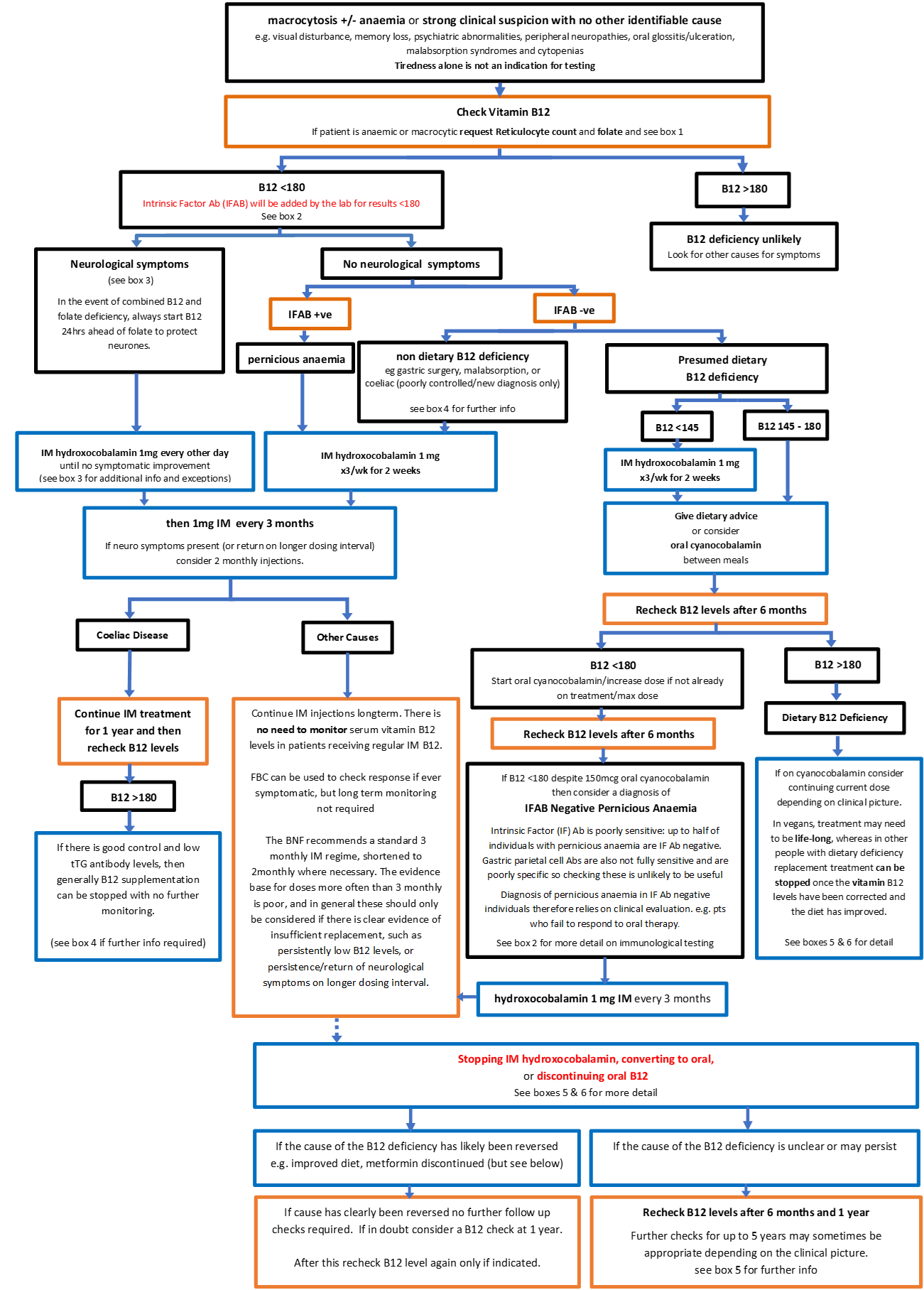
Box 1 – Notes on starting treatment in individuals with macrocytosis +/- anaemia
- If patient is anaemic or macrocytic request Reticulocyte count and folate to help differentiate causes and as a baseline for assessing immediate response to treatment.
- Note that in severe B12 or Folate deficiency supplementation may cause severe hypokalaemia as red cell reproduction restarts and a U&E check after starting treatment may be appropriate
- Check reticulocyte count again within 7–10 days of starting treatment if initial Haemoglobin and reticulocytes low. An increase in the reticulocyte count to above the normal range indicates that treatment is having a positive effect and red blood cell production is appropriately increasing.
- Repeat FBC and reticulocyte count at 8 weeks. The mean cell volume (MCV) should be normalising, and reticulocyte count rising. If reticulocyte count still low see refhelp macrocytosis guideline as may need haem referral
Example reticulocyte ranges:
Low < 25 (often seen in low B12/folate)
Normal 25-85
Raised > 85
Box 2 – B12 deficiency and immunological testing.
Traditionally, two immunological tests have been associated with assessing B12 status, but they are both potentially problematic:
- Intrinsic Factor antibody (IFAB) is poorly sensitive: IFAB may be absent in up to 40-50% of patients with pernicious anaemia, but positive IFAB is highly specific for pernicious anaemia.
- Gastric Parietal Cell Antibodies are also not fully sensitive and are poorly specific so checking these is not always useful. Please note that if you do order gastric parietal cell antibodies, they form part of a linked test array, so your patient will automatically also be tested for anti-mitochondrial antibodies (AMA), Smooth muscle antibodies and LKM1 antibodies – which are all associated with autoimmune liver disease
In those who have low B12 levels, but no clear cause, the diagnosis of IFAB negative pernicious anaemia therefore relies on clinical evaluation e.g. patients who fail to respond to oral B12 therapy following adequate replacement over at least 6 months (where IM B12 is not immediately indicated for other reasons).
In an individual where pre-test probability for pernicious anaemia is high (e.g. an older woman with a history of autoimmune diseases) a negative IF antibody result is more likely to be a false negative than in someone where pre-test probability is low (e.g. where there is an alternative explanation for B12 deficiency).
Box 3 – Notes on neurological symptoms and B12
- Neurological symptoms may be the only manifestation of B12 deficiency
- Symptoms include: lower limb sensory symptoms, suggestive of either a spinal cord lesion (subacute combined degeneration or peripheral neuropathy) or visual (optic neuropathy)
- People with B12 related sensory symptoms may especially have problems with proprioception and vibration loss
- Sensory symptoms are common in the normal population and modestly reduced B12 levels (e.g. 120 to 180pg/mL) are often “false positives” (i.e. there is no connection between the symptoms and result)
- People with mild or intermittent lower limb sensory symptoms, retained ankle reflexes or normal vibration sense at the toes are unlikely to have a B12 deficiency related neurological syndrome. Most such people, especially if symptoms are variable and intermittent, can be managed conservatively
- For people with mild sensory symptoms not responding to IM treatment it is unlikely that the symptoms were due to B12 deficiency. Consider alternative explanations and discontinue alt day IM treatment after 2 weeks. Maintenance may then be via the oral route unless there is a specific indication to give IM such as pernicious anaemia/ malabsorption
- B12 related neurological syndromes may occur with normal haematological indices (thus a normal B12 result may be a “false negative” result) although this is rare
- If combined B12 and folate deficiency always start B12 24 hours ahead of folate – Seek specialist advice only if symptoms are severe, there is diagnostic uncertainty and a neurology opinion is required to help determine the cause.
- B12 neurological symptoms typically take several months to improve and may not recover completely even with replacement. We suggest waiting at least 3 months for a clinical response.
Box 4 – Notes on Gastrointestinal Conditions and B12
Coeliac Disease
Adults
- Vitamin B12 levels should be measured at time of diagnosis of Coeliac Disease.
- Low B12 levels are likely to be secondary to malabsorption and should improve with gluten exclusion. However, Intrinsic Factor should be checked (done automatically by lab if B12 low) and an assessment made to exclude Pernicious Anaemia, as a small number of people will have a dual diagnosis, not surprising as both are autoimmune conditions.
- In adults it is prudent to give intramuscular replacement initially, but then move to oral, or no, B12 supplementation once the anti-tTG has normalised.
- A small number of patients will have ongoing poor dietary compliance, with high Anti-tTG, and may need ongoing supplementation, some by injection.
Paediatrics
- Vitamin B12 levels should be measured at time of diagnosis of Coeliac Disease.
- Low B12 levels are likely to be secondary to malabsorption and should improve with gluten exclusion. However, Intrinsic Factor should be checked (done automatically by lab if B12 low) and an assessment made to exclude Pernicious Anaemia, as a small number of people will have a dual diagnosis, not surprising as both are autoimmune conditions.
- Lothian GI experience is that most results will be normal, and low in very few children with a new diagnosis.
- In children, with a few exceptions (see below) oral B12 supplements should be sufficient.
- Vitamin B12 levels are re-measured at a year from diagnosis, and if normal, and there is good control and low tTG antibody levels, then generally B12 supplementation can be stopped.
- A small number of patients will have ongoing poor dietary compliance, with high Anti-tTG, and may need ongoing supplementation, some by injection.
- In children especially all these assessments and decisions would be made by the specialist GI service, and the GP advised accordingly.
Gastrointestinal Surgery
- Both gastrectomy and bariatric surgery can lead to B12 deficiency and require regular monitoring and replacement if levels are falling despite good dietary intake. Oral replacement is often inadequate in these patients since the cause is likely malabsorption.
- Patients who have undergone gastric bypass will require 3 monthly intramuscular injections of vitamin B12.
- Patients who have undergone sleeve gastrectomy surgery or duodenal switch are usually recommended to have initial 3 monthly intramuscular injections of vitamin B12 but may need less frequent injections depending on blood results, however, they should always be given IM rather than oral treatment.
- Terminal ileum resection is an indication for lifelong intramuscular B12 replacement
BOX 5 – Notes on either switching from IM to oral treatment OR discontinuing B12
- Individuals with pernicious anaemia or significant neurological symptoms with a clear response to IM B12 treatment should usually continue on IM B12 treatment lifelong
- NHS Lothian policy is for lifelong IM B12 for those who have had bariatric surgery.
- B12 liver stores may last anything from 1 – 11 years, although the consensus suggests 2-4 years, so for individuals previously on B12 treatment it may take a few years for their liver B12 stores to become depleted after treatment cessation.
- Upon treatment discontinuation or a switch from IM to oral treatment it is therefore important to consider whether or not it is appropriate to recheck B12 levels after 6 months, and potentially annually for up to 5 years to allow time for liver stores to become depleted.
- How essential this is depends on how likely is is that the patient may have undiagnosed pernicious anaemia or another malabsorptive state meaning that over time their B12 levels will once again become depleted. So for individuals where there is a history of malabsorption, other autoimmune diseases etc this monitoring is more important and the full 5 years of checks would be recommended
- Alternatively for individuals where there has been a clear dietary cause which has now resolved e.g. the patient has discontinued a vegan diet, supplementation can usually be stopped without any further monitoring. This will also apply to many where metformin was identified as a cause, with borderline low levels, and all other tests normal.
BOX 6 – Medication/conditions that may affect levels Vitamin B12
Metformin (for longer than 12 months)
- No need to routinely check levels for those with diabetes or on metformin
- Usually improved with dietary improvement of B12 intake
- It has been suggested that an increased intake of calcium reverses the vitamin B12 malabsorption induced by metformin. Bauman WA et al, Diabetes Care 2000 (23) 1227-31
- Only assess B12 levels if objective evidence of deficiency is present including peripheral neuropathy or macrocytic anaemia
- If low levels check IFAB and should be treated with a short course of OTC oral cyanocobalamin (50micrograms orally for 4 weeks). Response should be assessed clinically and continued if benefit is shown
- No need for prophylactic B12 administration
Proton pump inhibitors and H2 antagonists
- OTC oral replacement (25-100 micrograms orally) may be appropriate if objective evidence of deficiency is found
Anticonvulsants
- If no objective features of B12 deficiency- no need for replacement • OTC oral replacement (25-100 micrograms orally) may be appropriate if objective evidence of deficiency is found
Oral contraceptives and hormone replacement therapy
- Pregnancy and COCP cause altered B12 binding to plasma protein, so borderline/low levels are commonly seen, which may not indicate true deficiency
- Only assess B12 levels if objective symptoms develop and this is the only indication for treatment
- OTC oral replacement (25-100 micrograms orally) may be appropriate if objective evidence of deficiency is found
Colchicine
- Low levels can easily be increased with dietary supplementation
Antibiotics
- Low levels can easily be increased with dietary supplementation
Pregnancy
- Pregnancy and COCP cause altered B12 binding to plasma protein, so borderline/low levels are commonly seen, which may not indicate true deficiency
- B12 is not routinely measured during pregnancy, therefore only test if symptoms develop (as per protocol above for non-pregnant patients)
- If pregnant or breastfeeding it is recommended that cyanocobalamin is prescribed rather than over-the-counter
Vegetarian and vegan diets
- Vegetarians and vegans are at increased risk of B12 deficiency, especially during pregnancy and when breastfeeding. If relevant symptoms develop consider testing B12 levels, and oral supplementation may be required as per above protocol. If felt appropriate oral supplementation could be over the counter (NB: please provide the patient with instructions for what dose of cyanocobalamin to take as OTC supplements vary widely). However if pregnant or breastfeeding it is recommended that cyanocobalamin is prescribed.
C.M. & A.K. 15-03-23
This document outlines appropriate referrals to the haematology department. Please also see B12 Primary Care Management for FAQs on a wide range of clinical scenarios.
Primary care investigations
FBC and film.
Serum ferritin.
Serum folate.
Intrinsic factor antibodies.
Please also see macrocytosis/macrocytic anaemia/ cytopenia guidelines, if relevant.
Services
Patients may be referred to Department of Haematology RIE, WGH or SJH
Who to refer:
Patients not responding haematologically to B12 replacement therapy (where folate and iron stores have been checked and are normal).
Patients with suspected malabsorption or disease of the terminal ileum should be referred to Gastroenterology.
Patients with neurological symptoms should be discussed with Neurology if advice required.
Who not to refer:
Uncomplicated B12 deficiency
How to refer:
SCI Gateway Haematology
Thanks to the Vegan Society for allowing us to link to their website
https://www.vegansociety.com/resources/nutrition-and-health/nutrients/vitamin-b12
Devalia V et al (2014) Guidelines for the diagnosis and treatment of cobalamin and folate disorders https://onlinelibrary.wiley.com/doi/full/10.1111/bjh.12959 [Accessed 29.11.19]
Linnebank et al (2011) Antiepileptic drugs interact with folate and vitamin B12 serum levels https://onlinelibrary.wiley.com/doi/pdf/10.1002/ana.22229 [Accessed 22.10.19]
Sukumar and Saravanan (2019) Investigating Vitamin B12 deficiency https://www.bmj.com/content/365/bmj.l1865 [Accessed 29.11.19]













