Services
RIE: Dr Tracey Bradshaw
WGH: Dr Peter Reid
St John’s: Dr Donald Noble
Diagnosis of asthma
When to consider a diagnosis of asthma;
- Has the patient had an attack, or recurrent attacks of wheezing?
- Does the patient have a troublesome cough at night?
- Does the patient have a wheeze or cough after exercise?
- Does the patient have wheeze, chest tightness, or cough after exposure to airborne allergens or pollution?
- Do the patient’s colds go to the chest or take more than 10 days to clear up?
- Are the symptoms improved by appropriate anti-asthma treatment
How to diagnose asthma
Consider the diagnosis if the patient has 1 or more of the following;
Symptoms
- Wheeze
- SOB
- Chest tightness
- Cough
Signs
- None (common)
- Wheeze
- Tachypnoea
Helpful additional information
- Symptoms worse at night and/or early morning
- Personal or family history of asthma or atopy
- History of worsening after use of NSAIDs or β blockers
- Recognised triggers- e.g. allergens, cold air, exercise
Objective measurements that can be performed in primary care
- 20% diurnal variation on 3 or more days in a week for 2 weeks on PEF diary
or - FEV1 ≥ 15% (and 200mls) increase after short acting β2 agonist (e.g. Salbutamol 400mcg by pMDI + spacer or 2.5mg by nebuliser)
or - FEV1 ≥ 15% (and 200mls) increase after trial oral steroids (prednisolone 40mg/day for 14 days)
Using FEV1 or PEF as a response to treatment is of limited value in patients with near/normal lung function. Assess symptomatic response to treatment using a validated tool e.g. Asthma Control Test
Who to refer:
- Diagnosis unclear or in doubt
- Spirometry or PEF not appropriate to clinical picture
- Suspected occupational asthma- refer Dr Reid
- Patients who remain symptomatic and/or have impaired lung function and/or frequent exacerbations despite treatment at Step 4 BTS/SIGN Guidelines
- Previous life-threatening or near-fatal attack (How to recognise patients at-risk of near-fatal asthma)
Who not to refer:
- Mild intermittent, or mild to moderate persistent asthma who are well controlled unless any features documented above
How to refer:
- Use Gateway to refer to these services
- Dictation Checklist
- FEV1 or PEF if spirometry not available
- assessment of adherence (prescription records for asthma medications over past 12 months)
- CXR
Factors contributing to difficult to control asthma
1. Non adherence
2. Aggravating factors
- smoking
- obesity
- ongoing allergen exposure
3. Comorbidities
- psychological factors
- rhinosinusitis
- sleep apnoea
- bronchiectasis
Advice on sub-optimally controlled Asthma
- Clarify diagnosis
- Search for remedial aggravating factors that may be remedial (see notes below)
- Establish adequate inhaler technique
- Establish adherence to therapy
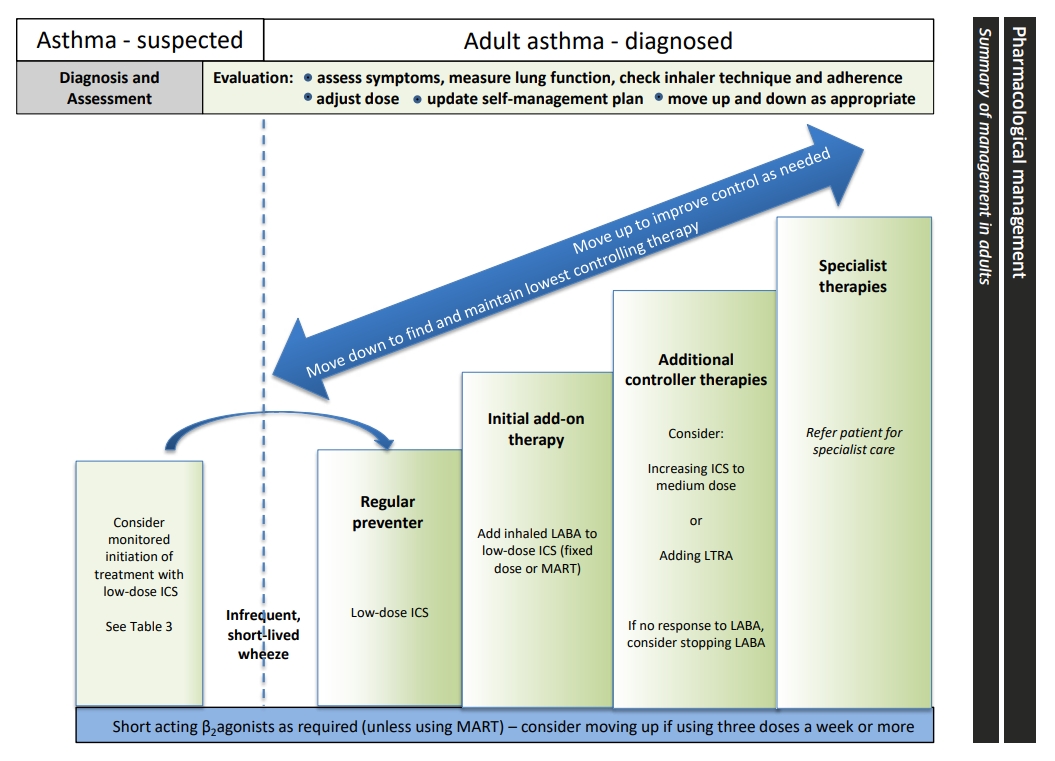
- Consider changing pharmacotherapy appropriate to BTS strategy: figure 4 Stepwise Management of Asthma (see below)
- Refer specialist advice.