Chronic spontaneous urticaria +/- angioedema (CSUA) – including in the context of Long Covid.
Definitions
The most common clinical manifestations of histamine release / mast cell degranulation are acute / episodic urticaria (weals) or skin itch, angioedema; and less commonly acute vomiting, abdominal pain and anaphylaxis. Therefore, the diagnosis of mast cell / histamine release mediated conditions relies primarily around clinical history.
Scope
This is a brief guide aimed at Primary Care providers on the approach to diagnosis and management of patients with symptoms of chronic urticaria (weals) +/- angioedema, occurring daily / almost daily for a period lasting > 6 weeks (some patients may be affected by symptoms occurring intermittently over months or years). Allergic urticaria/ angioedema and angioedema due to C1 inhibitor deficiency are outside the scope of this brief guidance note. This does not replace more detailed information provided by NICE and the BSACI guidance on chronic urticaria and angioedema.
Allergic urticaria and angioedema are usually identified by a clinical history of a temporal relationship of symptoms in relation to a particular food / trigger, by either ingestion or contact. Most episodes of urticaria are not allergic. More information on investigating isolated angioedema (i.e angioedema without weals) symptoms can be found in complement testing section at Immunology (nhslothian.scot) and is not covered in detail here – please also refer to the BSACI guidance on chronic urticaria and angioedema.
Anecdotally, many patients with Long Covid have described concomitant symptoms of urticaria and angioedema. It is well recognised that intercurrent infection or post viral illnesses can serve as triggers and exacerbators of urticaria and angioedema symptoms. Understanding the natural course of these symptoms in the context of long Covid, specifically, requires further research. Currently, there is no evidence to suggest that these symptoms arising in the context of long Covid should be managed any differently.
This guidance note does not serve to advise around referral pathways for patients requiring secondary care input, which will vary regionally across Scotland.
Introduction
Urticaria and angioedema is identified clinically. Images of typical appearances are available via the links below:
Chronic urticaria (+/- angioedema) affects 2-3% of the population and significantly reduces quality of life. Early recognition of symptoms and instigating treatment is recommended.
Triggers and exacerbators of CSUA
CSUA is not caused by an allergy.
Common recognised triggers of CSUA symptoms include infections (especially viral infection), psychological stress, and NSAIDs medications. There is also an association with hormone fluctuations (e.g association with oral contraceptive pill use in some women), and thyroid autoimmune disease. For many individuals, however, symptoms are largely idiopathic.
The natural history of CSUA is that for most individuals, symptoms ‘burn out’ with time (6-12 months). For ~20% of individuals with CSUA, they remain symptomatic for many years, and some may require specialist referral.
Treatment in CSUA
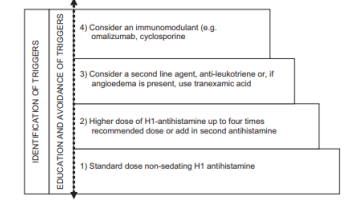
Treatment is based around symptom control, mainly by anti-histamine therapy which may need to be titrated up to 4 times the standard recommended doses to achieve symptom control. The figure below is inserted from the BSACI guideline.
Step 4 in the figure below would normally be applicable to secondary care management.
Mast Cell Activation Syndrome (MCAS
MCAS has been characterised by episodic signs and symptoms of systemic anaphylaxis / symptoms associated with mast cell degranulation that concurrently affect at least two organ systems.
Due to the broad range of possible symptoms affecting many organs, the MCAS diagnostic label may be used to inappropriately ascribe many symptoms to, e.g fatigue, rashes of many sorts, chronic illness, oedema, adenopathy, tinnitus, ‘brain fog’ and many others – all of which are not associated with mast cell / histamine induced symptoms. In addition, many symptoms which can less commonly be associated with histamine release e.g flushing and diarrhoea may be more chronic rather than episodic, which again would point towards other underlying diagnoses. This can cause marked uncertainty for patients and indeed lead to mis-diagnosis.
In some forums / groups, certain disorders have been used to diagnose MCAS with no scientific basis / evidence for any association with mast cell activation. Such conditions include Ehlers-Danlos syndrome, postural orthostatic tachycardia syndrome (POTS), sclerosing mediastinitis, psychiatric and other idiopathic disorders and others.
A detailed consensus document on MCAS can be found at AAAAI Mast Cell Disorders Committee Work Group Report: Mast cell activation syndrome (MCAS) diagnosis and management (2019)
Summary
The clinical characterisation of a patient’s symptoms in terms of urticaria / angioedema / CSUA is much more useful, clinically, and helps tailor effective treatment more specifically for the patient. In the context of long Covid / the Covid 19 pandemic, it would be reasonable to expect that more individuals will present with symptoms of urticaria, angioedema and idiopathic anaphylaxis – all of which can be precipitated and associated with infections, as well as any other acute or prolonged physiological or psychological stresses.
C.M & C.C 09-01-25
NHS Scotland www.dermatology.nhs.scot/dermatology-pathways/pathways/urticaria/
Patient information leaflets on CSUA are available at the links below:
British Association of Dermatologists PIL on urticaria and angioedema
Urticaria and Angioedema | Information on Hives | Allergy UK













