There is helpful, patient-friendly information and advice to be found on the GI section of the NHS Lothian Internet pages. There are also some videos by our very own GI team which patients have been responding very positively to. Consider sharing the link with patients and/or carers.
https://services.nhslothian.scot/GI/Dyspepsia
Definition
Dyspepsia or “indigestion” is very broadly defined as recurrent upper abdominal pain, with or without bloating, nausea and vomiting. Symptoms are often exacerbated by eating and early satiety is a recognised feature.
Referral for endoscopy is seldom necessary in younger patients – cancer is exceptionally rare in patients under 55 with dyspepsia, in the absence of alarm symptoms. Some will respond to H. pylori eradication, some will benefit from acid suppression, but the majority will have functional dyspepsia (FD), a disorder of gut-brain interaction (DGBI), similar to IBS.
A test and treat strategy for H pylori should be adopted in the first instance if age <55 years
- See Primary Care Management for those aged <55 years
- However, age>55 years is an important determinant of more serious pathology
Updated Oct 25 IA, CN, LP & JB
Before considering referral for endoscopy
- Consider the age of the patient
- Serious pathology is rare in those <55 years with no alarm symptoms
- Undertake medication review to look for drugs which make cause or exacerbate symptoms
- NSAIDs
- Corticosteroids
- Opioids including codeine-based analgesia
- Calcium channel antagonists
- Nitrates
- Theophyllines
- Bisphosphonates
- Consider other diagnoses
- Gallstone or biliary disease (especially if severe, episodic pain)
- Cardiac disease
- In those who have had a previous endoscopy in last 3 years, but no new alarm symptoms, consider treatment in line with the results of that that previous endoscopy
- Normal endoscopy & USS- treat as Functional dyspepsia (FD)
- Previous oesophagitis-treat as GORD
- A test and treat strategy for H pylori should be adopted in the first instance if age <55 years
However, age>55 years is an important determinant of more serious pathology –PLEASE SEE BELOW
Guidelines for referral for Urgent Suspected GI Cancer
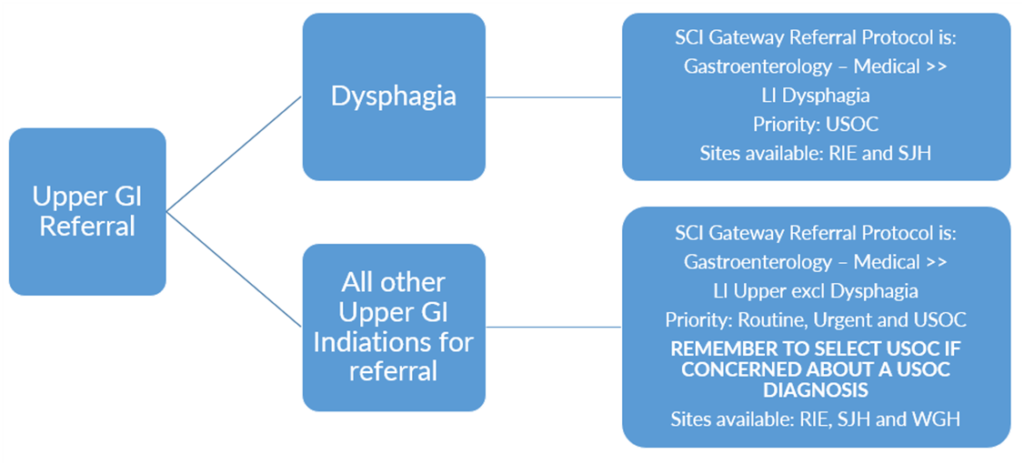
Upper GI USOC Referrals are divided into two referral pathways:
Summary of Upper GI Referral Pathways in NHS Lothian
In the absence of alarm symptoms in those aged <55 years:
Consider lifestyle measures
- Achieve and maintain healthy weight, take regular aerobic exercise, avoid food triggers, avoid smoking, reduce caffeine intake, modify alcohol intake. No evidence to support diet therapy e.g. low FODMAP.
Trial of alginates as required
Offer trial of an H2RA (Famotidine 20-40mg OD)
If no response to simple measures, then either:
- Test and treat Helicobacter pylori
- Check H pylori stool antigen and treat if positive
- Stop PPI for at least 2 weeks prior to test
- See LJF for H pylori treatment regimens
or
- Treat with full dose PPI (omeprazole 20mg-40mg od or equivalent) for 4 weeks
- If symptoms recur offer ongoing PPI therapy but step-down treatment to lowest effective dose as there is no real dose-response effect in dyspepsia
- Discuss use of “as required” treatment to encourage self- management of symptoms
- Offer annual review to assess symptom control and reduce or withdraw treatment if possible
Further information
Management of those with normal investigations (Functional dyspepsia)
- Secondary Care would consider using the following measures:
- If still symptomatic despite above measures, offer low-dose tricyclic agent (TCA) as a gut-brain neuromodulator e.g. nortriptyline or amitriptyline 10-20mg at night, titrated slowly up to 30-50mg nocte, as required and tolerated. Careful explanation of the rationale is required as is counselling about side-effects
- Mirtazapine 15mg OD can be effective in FD when there is early satiation and weight loss
- These are unlicensed uses and not listed on the formulary for these indications. Referrers can use SCI Gateway to seek Specialist advice however, if they think this would be an option that would be helpful for a patient.
- Gut-brain directed behavioural therapies including stress management, CBT, hypnotherapy can be useful in some patients. There is currently no facility for this in NHS Lothian in primary or secondary care.
- No evidence to support the use of either SSRI or SNRI drugs in FD
Dyspepsia and Gastro Oesophageal Reflux Disease (NICE 2014, update 2019)
BSG guidelines (2023) on management of functional dyspepsia:
www.bsg.org.uk/clinical-resource/bsg-guidelines-on-the-management-of-functional-dys













