Key messages
Iron deficiency anaemia is defined as a low haemoglobin in the presence of either:
- Low ferritin <30 (best diagnostic marker)
- Low serum iron in the presence of transferrin >3.0
The prevalence of iron deficiency anaemia amongst adult males and non-menstruating females in the developed world is 2-5%
Iron deficiency anaemia can arise as a consequence of:
- Loss of iron (menstruation, GI tract, renal tract)
- Malabsorption (previous gastric surgery, Coeliac disease)
- Poor dietary iron intake (poor diet, lifestyle choices or cultural beliefs) may be contributing factors.
Key factors in assessment:
- Menstrual blood loss is the commonest cause overall
- Testing for Coeliac disease (anti tTG antibodies) is important
- Urinalysis to detect renal tract blood loss should be performed in all patients with IDA, but if positive the patient should still be referred along the GI IDA pathway. However, it should be noted on the SCI Gateway referral form, so GI are aware of this.
- NOTE THAT IRON AND TRANSFERRIN SHOULD BE DONE ON A FASTING SAMPLE
Updated Oct 25 IA, CN, LP & JB
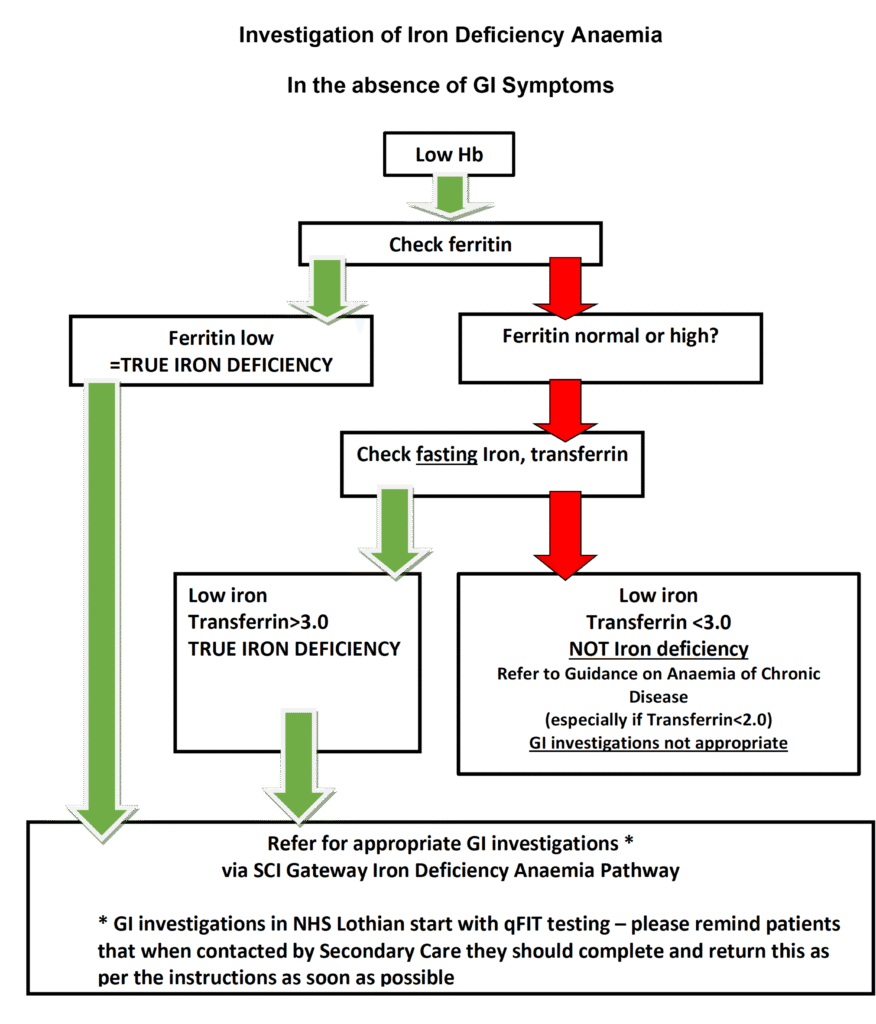
These individuals should be referred for appropriate GI investigations if they are sufficiently fit to undergo them, understand what investigations will mean for them and wish to be investigated.
GI investigations in NHS Lothian start with stool qFIT testing: please remind patients that when contacted by Secondary Care they should complete and return this as per the instructions as soon as possible. Please see the After Referral section below for further information on what happens next.
Referral protocol available via SCI Gateway as follows:
- RIE >> Gastroenterology – Medical >> LI Iron Deficiency Anaemia
- SJH >> Gastroenterology – Medical >> LI Iron Deficiency Anaemia
- WGH >> Gastroenterology – Medical >> LI Iron Deficiency Anaemia
The referral protocol asks the following questions / for the following tests:
- Has the Hb been tested?
- Has Ferritin been tested?
- Is Ferritin low?
- Have FASTING Iron and Transferrin been tested?
- Is Iron low?
- Is Transferrin >3.0?
- Has Coeliac testing been carried out?
- Is the patient diabetic?
- Have Cr+Es been done in the past 4 weeks?
(Both of the above questions asked in case triaged to investigation requiring contrast)
- Urinalysis results
- Is Key Information for Endoscopy available (e.g. anticoagulation; prosthetic heart valve; diabetic on insulin; severe comorbidity: full details should be noted in the Referral Text)
- Menstrual history (where appropriate)
- Past Medical History of Gastric Surgery (indication and operation) (where appropriate)
- Family History
After Referral
GI investigations in NHS Lothian start with stool qFIT testing: please remind patients that when contacted by Secondary Care they should complete and return this as per the instructions as soon as possible .
Investigation of the upper and lower GI tract will be undertaken, using the stool qFIT testing to stratify risk and guide the sequence (upper or lower GI first) and timing (USoC or urgent or routine) of tests:
- Upper GI Endoscopy combined with either
- Colonoscopy or CT colonography or minimal preparation CT scan*
Appropriate investigation will be at the discretion of the secondary care team and will depend on a patient’s age and general fitness (which may have to be determined by clinic visit first)
- CT colonography will be offered to less fit patients or those who cannot tolerate colonoscopy
- As above FBC, U&Es and LFTs (where possible) should be taken prior to referral in order to expedite further investigations. These investigations should have been taken within 4 weeks of referral
- Minimal prep CT (no purgative laxative preparation) will be reserved for the most frail patients where any investigation at all is appropriate*
As Menstruation is the most common cause of IDA in menstruating people under 50 years of age, then this group of patients can still be referred under the IDA Referral pathway, but they will be triaged to stool qFIT testing only, and if double qFIT testing is negative they will not proceed to other GI investigations
GI investigations may be appropriate for patients >50 years (and without history of menorrhagia) with proven iron deficiency in the absence of anaemia.
If all investigations are negative, but the patient has been noted to have blood present on urinalysis, then at this point referral along the Non Visible Haematuria pathway may be appropriate.
GI investigations are not appropriate in other types of anaemia unless there are clear GI symptoms to be investigated.
Please see guidance on the Haematology Iron Deficiency Anaemia page for guidance on managing Iron Deficiency Anaemia













