Bronchiectasis is defined as having inflamed, permanently and irreversibly damaged and dilated airways leading to symptoms of chronic cough, chronic sputum production and recurrent respiratory tract infections.
The disease is life-long, and the prognosis depends on the severity of the bronchiectasis. In severe cases, life expectancy will be reduced.
Patients chronically colonised with Pseudomonas aeruginosa tend to have poorer health related quality of life, more exacerbations and increased mortality.
Refer all patients suspected of having bronchiectasis. Please let the patient know that they are likely to receive an appointment for a CT scan of their chest (looking for radiological signs of bronchiectasis) in advance of their clinic appointment.
Royal Infirmary of Edinburgh (Lead Centre) – Dr Anna Lithgow
St John’s Hospital – General Respiratory Physician
Western General Hospital – General Respiratory Physician
Definition of Severity
The Bronchiectasis Severity Index (BSI) may also be used to define severity of bronchiectasis. The table below documents the variables within the BSI index and its scoring system. A total score 0 – 4 indicates mild disease, 5 – 8 moderate disease and ≥ 9 severe disease. The BSI can be used as an adjunct when assessing a patient and deciding on their management.
Variables involved in calculating the severity score in the Bronchiectasis severity index
| Factor and points for scoring system | | | | |
| Age (years) | <50 (0 points) | 50-69 (2 points) | 70-79 (4 points) | >80 (6 points) |
| BMI (Kg/m2) | <18.5 (2 points) | 18.5-25 (0 points) | 26-30 (0 points) | >30 (0 points) |
| FEV1% predicted | >80 (0 points) | 50-80 (1 point) | 30-49 (2 points) | <30 (3 points) |
| Hospital admission within last 2 years | No (0 points) | Yes (5 points) | ||
| Number of exacerbations in previous 12 months | 0 (0 points) | 1 – 2 (0 points) | ≥3 (2 points) | |
| Modified MRC breathlessness score | 0-2 (0 points) | 3 (2 points) | 4 (3 points) | |
| P. Aeruginosa colonisations | No (0 points) | Yes (3 points) | ||
| Colonisation with other organisms | No (0 points) | Yes (1 point) | ||
| Radiological severity | <3 lobes affected(0 points) | ≥3 lobes of cystic bronchiectasis in any lobe (1 point) | ||
0-4 point s =mild disease; 5–8 = moderate disease; 9 and over = severe disease The BTS Guideline for Bronchiectasis in Adults, BTS (2019)
Who to refer:
Suspected bronchiectasis – new referral
- Patients with persistent cough productive of mucopurulent or purulent sputum.
- ≥ 2 chest infections in the past year with evidence of positive sputum bacterial cultures
- Patients with COPD who have had their treatment optimised but still have a chronic productive cough with positive sputum bacterial cultures whilst stable, or have had 2 or more exacerbations with positive sputum bacterial cultures in the preceding 12 months.
Please let the patients know that they are likely to receive an appointment for a CT scan of their chest (looking for radiological signs of bronchiectasis) in advance of their clinic appointment.
For mild cases, care will be in the community. For severe cases, care will be with regular hospital review.
For new cough (no known pathology) greater > 3 weeks think Detect Cancer Early (DCE) pathway
Known bronchiectasis – indications for re-referral
- Patients with chronic Pseudomonas aeruginosa, non-tuberculous mycobacteria (NTM) or methicillin-resistant Staphylococcus aureus colonisation (MRSA)
- Deteriorating bronchiectasis with declining lung function
- Recurrent exacerbations (≥3 per year)
- Haemoptysis: new or unusual. Large volumes (>10 mls over 24 hours) will need emergency admission.
- Patients receiving long term antibiotic therapy (oral, inhaled or nebulised)
- Patients with bronchiectasis and associated rheumatoid arthritis, immune deficiency, inflammatory bowel disease, primary ciliary dyskinesia and allergic bronchopulmonary aspergillosis (ABPA)
- Patients with advanced disease and those considering transplantation.
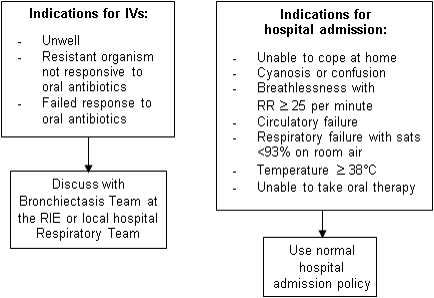
Indications for IV antibiotics and hospital admissions
Who not to refer:
- Patients with occasional LRTI and an already established respiratory disease
How to refer:
- Refer via SCI-Gateway (Respiratory)
- Recommended investigations:
- sputum culture (commonly Haemophilus influenzae, Moraxella catarrhalis, Staphylococcus aureus, Streptococcus pneumoniae and Pseudomonas aeruginosa)
- CXR (a normal CXR does not exclude bronchiectasis)
If a CXR shows radiological signs of lung cancer, then refer URGENTLY via lung cancer pathway.
Structured Secondary Care Letters
Secondary care clinic letters, from the RIE outpatient settings are structured. The first section contains the most relevant information for primary care. The second section includes further background information.
- Diagnosis
- Recommended antibiotic for exacerbation
- Radiology – CT scan result
- Plan, Investigations and Follow-up
- For GP: please consider KIS e.g. recommended antibiotics for exacerbations, current O2 sats, last FEV1, whether on long-term antibiotics, usual level of breathlessness if present
- Long Term Antibiotics
- Date of last IV antibiotics/hospital admission
- Number of antibiotic courses since last assessment
- Weight/BMI
- Spirometry and O2 saturations
- Sputum production and sputum colour
- Whether chronically colonised
- Microbiology since last seen
- Current Medication
- Bronchiectasis status – stable or exacerbation
Further background information
- Date of bronchiectasis diagnosis
- Smoking history
- Presence of rhinitis/GORD
- Usual and previous sputum pathogens
- Whether performing regular chest physiotherapy
- Annual flu vaccination and pneumococcal vaccination status
- Last CT chest scan and CXR results
- Results of previous relevant investigations e.g. immunology, aspergillus, echo
Resources
- Hill AT, Sullivan AL, Chalmers JD, et al. BTS Guidelines for Bronchiectasis in Adults. Thorax 2019; 74 (Suppl 1):1–69
- Gruffydd-Jones, K., Keeley, D., Knowles, V. et al. Primary care implications of the British Thoracic Society Guidelines for bronchiectasis in adults 2019. npj Prim. Care Respir. Med. 29, 24 (2019)
Cornerstone of Bronchiectasis Management in Primary Care
- Self-management advice for patients is available on the NHS Lothian Patient Bronchiectasis website: www.bronchiectasis.scot.nhs.uk. Patient should also have a personalised bronchiectasis self-management plan booklet.
- Consider a KIS which can include the following information: recommended antibiotics for exacerbations, current O2 sats, last FEV1, whether on long-term antibiotics and usual level of breathlessness if present.
- Encourage chest physiotherapy (chest clearance) once or twice per day and increase during bronchiectasis exacerbations. Direct patients to www.bronchiectasis.scot.nhs.uk for a reminder on chest clearance techniques.
- Recommend annual flu vaccinations.
- For bronchiectasis exacerbations/chest infections send a sputum sample for routine bacterial culture and start prompt antibiotics (don’t wait until the sputum cultures are available). This should be for 14 days (7 days may suffice in mild bronchiectasis).
- Antibiotics for exacerbations of bronchiectasis should (if possible) be based on previous sputum pathogen/s and sensitivities. If there are no previous sputum pathogen/s or sensitivities, below are the recommended antibiotics and doses for common sputum organisms found in bronchiectasis.
Recommended antibiotics and doses for common sputum pathogens found in bronchiectasis.
| Sputum Pathogen | Antibiotics (14 days) |
| Haemophilus Influenzae β-lactamase negative | Amoxicillin 500mg TDS or clarithromycin 500mg BD |
| Haemophilus Influenzae β-lactamase positive | Co-amoxiclav 625mg TDS or doxycycline 100mg BD |
| Moraxella catarrhalis | Co-amoxiclav 625mg or doxycycline 100mg BD |
| Streptococcus pneumonia | Amoxicillin 500mg TDS or clarithromycin 500mg BD |
| Staphylococcus aureus | Flucloxacillin 500mg QDS or clarithromycin 500mg BD |
| Pseudomonas aeruginosa | Ciprofloxacin 500mg BD |
| Methicillin-resistant Staphylococcus aureus (MRSA) | Doxycycline 100mg BDIf there is no response or the patient is unwell then refer to secondary care for IV antibiotics |
Please see separate flowcharts for management advice on the following:
- Guidelines for Managing Individual Chest Infections
- Guidelines for Managing Recurrent Chest Infections
- Managing Mild to Moderate Non-CF Bronchiectasis
For further questions please see Frequently Asked Questions in Bronchiectasis
All above guidelines are recommendations of best practice based on the latest National Guidelines for Bronchiectasis 2019.
- Guideline for diagnosis and treatment of adult bronchiectasis
- Lothian Bronchiectasis Website (www.bronchiectasis.scot.nhs.uk
- Primary care implications of the British Thoracic Society Guidelines for Bronchiectasis in Adult 2019
- Bronchiectasis Self-Management Plan
- Bronchiectasis Antibiotic/Infection Card (these are available from Kim Turnbull, Bronchiectasis Nurse Specialist, RIE)
- Lothian COPD Guidance April 2018 v0 4 Combined
- National Institute for Health and Care Excellence (NICE)
- Scottish Intercollegiate Guidelines Network (SIGN)
- BTS Guidelines for Bronchiectasis in Adults
- Respiratory-Frequently Asked Questions in Non-CF Bronchiectasis-April 2020
- Respiratory-Guideline for Managing Individual Chest Infections in Non-CF Bronchiectasis- April 2020
- Respiratory-Guideline for Managing Recurrent Chest Infections in Non-CF Bronchiectasis-April 2020
- Respiratory-Managing Mild to Moderate Non-CF Bronchiectasis – Respiratory Symptoms- April 2020
- Respiratory BRONC – Guideline for diagnosis and treatment of adult bronchiectasis (updated 23-09-2016)
- Respiratory BRONC Bronchiectasis.Scot (www.bronchiectasis.scot.nhs.uk)
- Respiratory BRONC Guideline for Non-CF Bronchiectasis (www.brit-thoracic.org.uk)













