A joint working group comprising representatives from the Association of Clinical Biochemistry, The British Thyroid Association and British Thyroid Foundation published on the ‘UK Guidelines for the Use of Thyroid Function Tests’. These give guidance on the optimal use of thyroid function tests (TFTs) to diagnose and monitor thyroid disease.
The following are suggestions for the use of thyroid function tests in Primary Care , derived from the UK guidelines, and modified to account for local practice.
PREVALENCE OF HYPOTHYROIDISM
Females
- In women, the prevalence of newly diagnosed overt hypothyroidism increases from 0.3% in younger women to 2% in women over 60 y.
- The prevalence of subclinical hypothyroidism (normal Free T4; high TSH) in women below 40y is approximately 4-6%, rising to 10-15% at 60y-75y.
Males
- In males the overall prevalence of overt hypothyroidism is low at <0.1% but for subclinical hypothyroidism the prevalence is approximately 10% for those over 60y.
SCREENING AND SURVEILLANCE– who to test?
- Screening in the healthy asymptomatic population is not warranted.
Symptomatic patients: –
- Patients with features of a thyroid disorder.
- Women at the menopause, when presenting with non-specific symptoms.
- Elderly with non-specific symptoms
Surveillance of ‘At Risk Patients’
| Patients stabilised on T4 | annual check* |
| Type 1 diabetes | annual check |
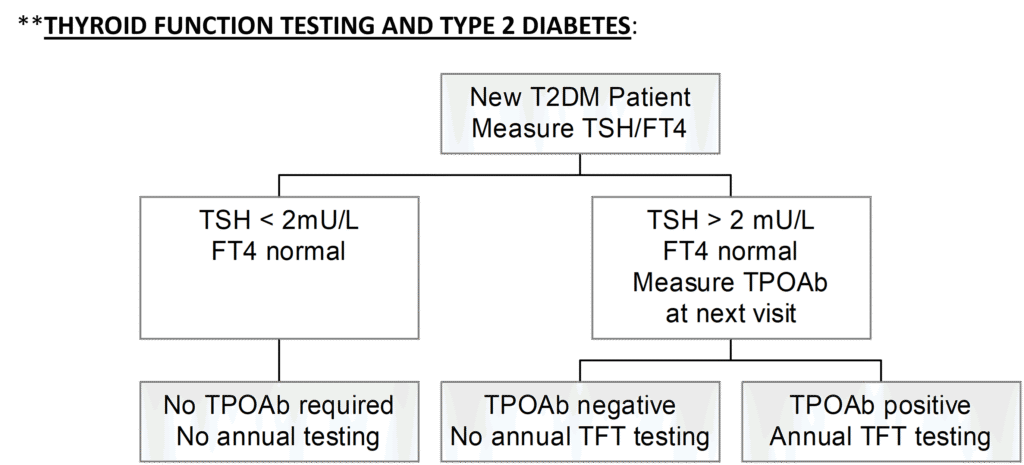
| Type 2 diabetes | at diagnosis; then annually only if TSH is >2.0mU/L & TPOAb +ve** |
| Treated hyperthyroidism | annual check |
| Downs and Turner’s syndrome | annual check |
| Post – neck irradiation | annual check |
| Post – partial/hemi-thyroidectomy | at 6 weeks and 6 months post-op; then annually |
| Lithium or Amiodarone | 6 monthly check |
* Conventional practice is to recheck TFTs on an annual basis in people on a stable dose of T4. Lothian general practice data suggests that the frequency of monitoring can be safely reduced to 2 years in patients on a stable dose of T4, but patients should be advised to have an earlier check of TFTs if they have any symptoms suggestive of thyroid dysfunction. However, women of reproductive age should continue to have an annual check of thyroid function because of the potential adverse risks of sub-optimally treated hypothyroidism in pregnancy.
HYPOTHYROIDISM – DIAGNOSIS AND MANAGEMENT
Overt Primary Hypothyroidism – (Free T4 low; TSH high – usually TSH > 20mU/L)
- Commence patient on T4 (if transient thyroiditis is excluded)
- Please also see separate advice on hypothyroidism in pregnancy.
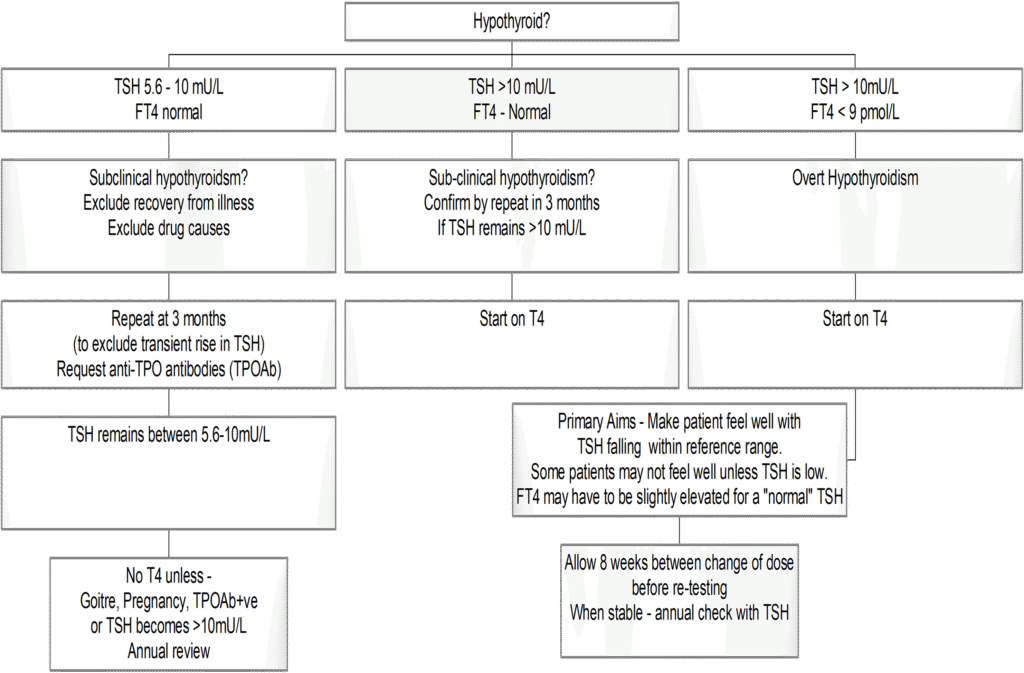
Subclinical Primary Hypothyroidism – (Free T4 normal; TSH high).
Many cases of sub-clinical hypothyroidism are transient. It is essential to confirm that abnormalities in TSH are persistent or progressive. Studies suggest that the average patient will not get any clinical benefit from T4 therapy until TSH rises above approximately 10 mU/L.
- Repeat TSH/FT4 at 3 months to exclude transient rise in TSH. Request anti-TPO antibodies to help to determine if an autoimmune process is present and help predict risk of progression to overt hypothyroidism.
If on repeat
- If TSH > 10 mU/L – start on T4
- If TSH lies between 5.6 – 10 mU/L, annual monitoring required.
Commence T4, when TSH subsequently becomes >10 mU/L. A trial of T4 may be warranted in a few patients eg if they are symptomatic with goitre or planning pregnancy (see below). Some endocrinologists may also commence T4 therapy if TPO Ab positive; this is because such patients have a greater risk of developing overt hypothyroidism.
Subclinical Hypothyroidism & Pregnancy
Women with sub-clinical hypothyroidism who are planning pregnancy or become pregnant should be advised to seek GP review for a check of thyroid function and TPO antibodies and consideration of levothyroxine replacement depending on their results. Please see the guidance on the management of subclinical hypothyroidism in pregnancy.
Levothyroxine (T4) REPLACEMENT
Aim – to make patient feel well and restore TSH and free T4 to within reference range. In some patients free T4 may have to be above the reference range to achieve a ‘normal’ TSH.
Some patients report they “feel better” only when T4 is given at a dose that produces a low or undetectable TSH. There have been some reports of decreased bone mineral density in postmenopausal women on T4 who have a TSH <0.1 mU/L. These studies are not conclusive and thus some endocrinologists will allow some patients to run with a low or undetectable TSH but only if T3 lies unequivocally within the reference range.
Monitoring
- Please use the tick box on GPOC / ICE for thyroxine monitoring
- When T4 dose is changed, a period of 2-3 months should elapse before re-testing.
- When a patient is stabilised on T4, TSH alone is required; the laboratory will automatically perform a free T4 if TSH is abnormal. This is only applicable to those patients who are “stable” on thyroxine. If the patient’s TFTs have been fluctuating or a previous test has shown an undetectable TSH, then TSH and Free T4 should be measured. Nurses leading an annual review clinic should be informed of the situations where both TSH and FT4 are required.
Medication and T4 therapy
- Some over-the counter medications can impair T4 absorption. These include: – PPIs and H2 antagonists, calcium carbonate, soy protein, aluminium hydroxide and ferrous sulphate.
- Do not take T4 within 4 hours of taking other medication.
- The requirement for T4 is likely to increase in hypothyroid patients who become pregnant or who are commenced on anticonvulsants or oestrogen containing oral contraceptives.
T3 replacement
T3 therapy is rarely required and there is no consistent evidence to recommend the use of combined therapy with T3 and T4. The aim of T3 therapy is to normalise TSH. Measurement of Free T4 is of no value in assessing patients on T3. Serum T3 measurements are of limited value due to the variability of T3 concentrations in blood after a T3 dose.
HYPOPITUITARISM and HYPOTHYROIDISM
Secondary hypothyroidism should be considered in patients presenting with low FT4 and normal (or only slightly raised) TSH. However, a low Free T4 in the presence of a normal TSH is most commonly due to non-thyroidal illness or the use of NSAIDs, furosemide, anticonvulsants or high dose glucocorticoids.
If hypopituitarism is suspected, an endocrinologist should carry out further investigation and assess the requirement for treatment.
Monitoring T4 therapy in hypopituitarism – Specialist Care
TSH measurements are of no value in monitoring these patients. An Endocrinologist should guide treatment and follow-up.
The aim of therapy is to maintain Free T4 in the upper half of the reference range (18-28 pmol/L).
C.M. & N.Z. 29-9-25
Who to refer:
Straightforward hypothyroidism can usually be managed in primary care, but endocrinology is happy to offer advice (select ‘Advice only’ on SCI Gateway) or see cases that may not be straightforward, for example:
- Hypothyroidism during or within 12 months of pregnancy (this may be a transient thyroiditis)
- Cases where there is diagnostic uncertainty
- History of neck pain, systemic upset or earlier thyrotoxic symptoms suggesting transient thyroiditis
- TSH <20, particularly if there is a suspicion of pituitary pathology
- Cases associated with amiodarone or lithium therapy
Who not to refer:
Patients with straightforward primary hypothyroidism with positive anti-thyroid peroxidase antibodies (or with subclinical hypothyroidism) and none of the features of diagnostic uncertainty highlighted in the ‘Who to refer’ section do not need further investigation or referral to endocrinology. Treatment with levothyroxine can be managed in primary care.
Advice can be requested using the ‘Advice only’ option on SCI Gateway.
How to refer:
By SCI Gateway to RIE / SJH / WGH Endocrinology.
The complete version of the UK Guidelines is available on the British Thyroid Association website:- ‘UK Guidelines for the Use of Thyroid Function Tests’.













