Who should get vitamin D supplementation?
The UK Scientific Advisory Committee on Nutrition recommends that everybody in the UK population should take a daily 400 unit (=10µg) vitamin D supplement, throughout the year.
Who should I check a vitamin D level on?
Patients with symptoms and signs of vitamin D deficiency.
Symptoms and signs of vitamin D deficiency:
- Bone pain
- ‘Growing pains’
- Muscle weakness
- Gross motor delay
- Poor growth
- Dental caries
- Symptoms of hypocalcaemia (seizures, tetany)
- Clinical signs of rickets (thickened wrists, genu varum, genu valgum, rachitic rosary, pectus carinatum, kyphoscoliosis, craniotabes, frontal bossing) or radiological features of rickets
- Bone biochemistry abnormalities found on incidental testing (e.g. incidental raised ALP)
Investigations / clinical assessment:
- 25-OH vitamin D
- Calcium, phosphate, U&Es and creatinine, LFTs, ferritin, FBC and PTH (iron deficiency anaemia and vitamin D deficiency often co-exist)
- Left wrist x-ray (specify ?rickets)
- Plot height& weight(and head circumference if <2 years)
Biochemical presentation of Vitamin D deficiency:
- 25-OH vitamin D – low
- Calcium – normal or low
- Phosphate – normal or low
- Alkaline phosphatase (ALP) – normal or high
- PTH – normal or high
Refer to current NHS Lothian Vitamin D Deficiency in Children for more details NHSL Guideline Template
D.R.M & C.H. 04-07-25
Who to refer:
- Normal vitamin D level and abnormal biochemistry and/or presence of rickets – discuss with Paediatric Endocrinology – see contact details section on Endocrinology & Diabetes (Paediatrics) – RefHelp
- If any deviation from the expected course during treatment of vitamin D deficiency, for example if unexpected abnormal results after treatment.
Who not to refer:
- Most children and young people with straight forward Vitamin D deficiency (i.e no suggestion of rickets or unexpected biochemistry results) can be managed safely in primary care (see Management flowchart under Primary Care Management tab)
- Elevated urea or creatinine – discuss with Paediatric Nephrology
- Elevated liver enzymes or suspected GI malabsorption – discuss with Paediatric Gastroenterology – see contact details section on Gastrointestinal – RefHelp
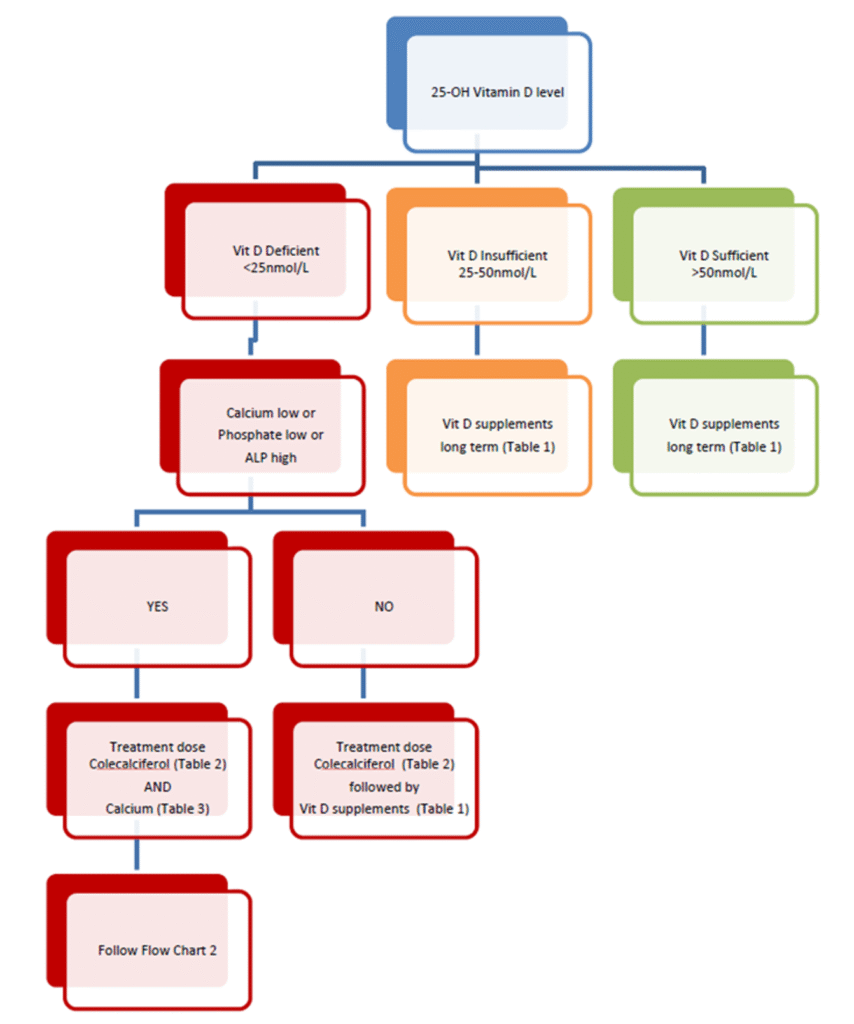
Management of Vitamin D deficiency: this is done in primary or secondary care
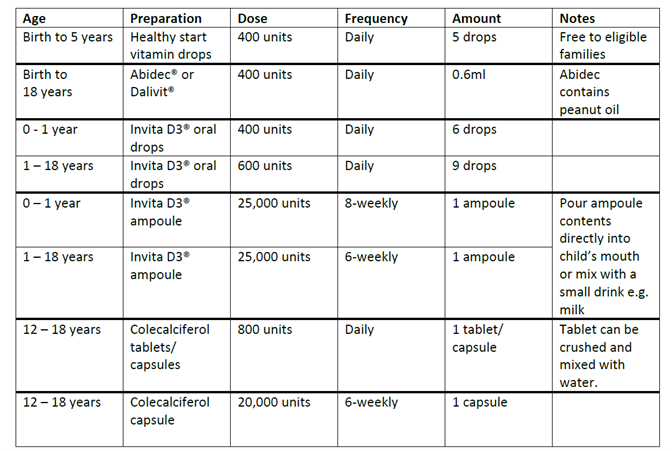
Prescription of Vitamin D supplements (Table 1):
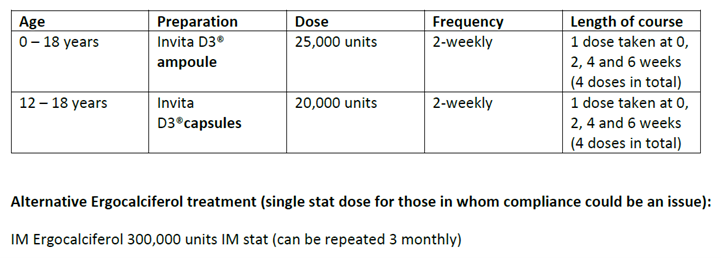
Cholecalciferol treatment (Table 2):
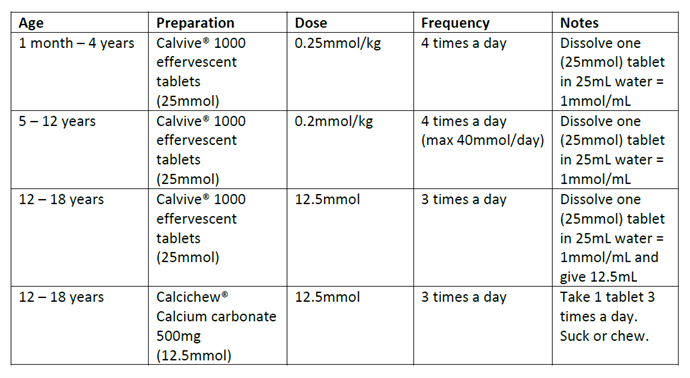
Calcium treatment (Table 3):
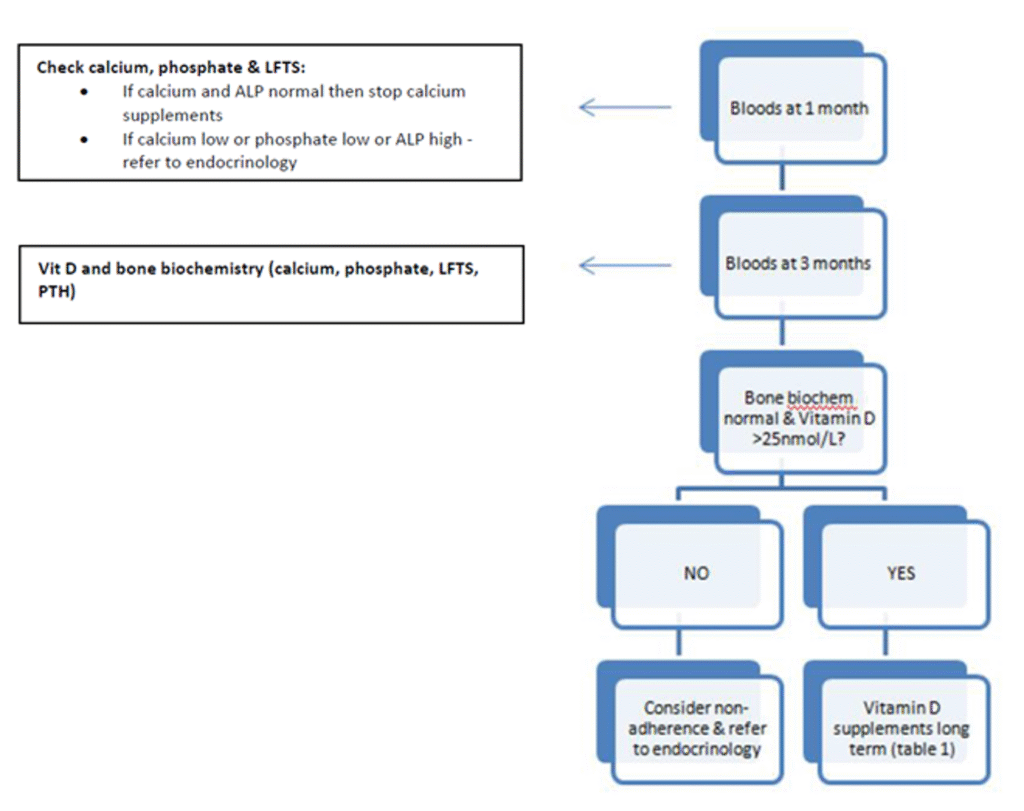
Monitoring (for patients with proven vitamin D deficiency commenced on cholecalciferol AND calcium):
NHSL Guideline Template (Vitamin D Deficiency in Children and Young People NHS Lothian guideline)
SACN vitamin D and health report – GOV.UK













