There is helpful, patient-friendly information and advice to be found on the GI section of the NHS Lothian Internet pages. There are also some videos by our very own GI team which patients have been responding very positively to. Consider sharing the link with patients and/or carers. Please note that although the relevant section is named “Dyspepsia” there is some relevance to GORD patients too.
https://services.nhslothian.scot/gi/dyspepsia
Symptoms of GORD:
- Heartburn
- Regurgitation of gastric contents into the mouth
- Waterbrash (excessive salivation)
- Chest pain
Diagnosis
The diagnosis of GORD is usually made on the clinical history. Typically patients will describe retrosternal burning (“heartburn”), often at night or on stooping. Up to half of reflux patients have atypical symptoms including upper abdominal pain, bloating, nausea/vomiting. The onset of symptoms is frequently associated with weight gain.
Updated Oct 25 IA, CN, LP & JB
Before considering referral for endoscopy / or oesophageal cell collection device (Cytosponge):
- Undertake medication review to look for drugs which make cause or exacerbate symptoms
- NSAIDs
- Corticosteroids
- Opioids including codeine-based analgesia
- Calcium channel antagonists
- Nitrates
- Theophyllines
- Bisphosphonates
- Consider alternative diagnoses including:
- Gallstone or biliary disease (especially if severe, episodic pain)
- Cardiac disease
- Normal endoscopy-treat as Functional Dyspepsia (FD)
- Previous oesophagitis-treat as GORD/oesophagitis
GORD is very common, affecting up to 20% of the adult population at any given time
Patients usually complain of a combination of
- heartburn (an uncomfortable burning sensation in the chest that often occurs after eating)
- acid reflux (where stomach acid comes back up into the mouth and causes an unpleasant, sour taste)
- bloating and belching
- nausea and/or vomiting
Referral for further tests is seldom necessary in younger patients
- See Primary Care Management for those aged <55 years
However, AGE (55 years or over) is an important determinant of pathology – PLEASE SEE BELOW
Guidelines for referral for Urgent Suspected GI Cancer
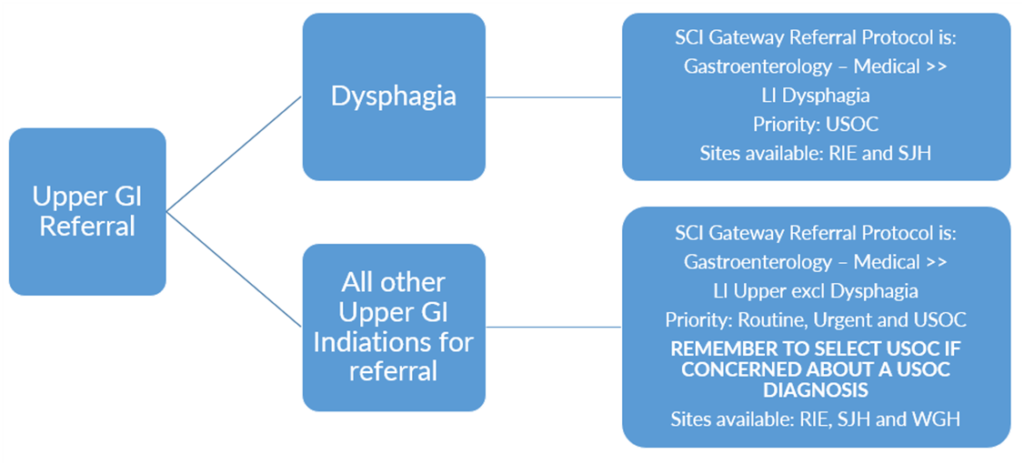
Upper GI USOC Referrals are divided into two referral pathways:
Summary of Upper GI Referral Pathways in NHS Lothian
In the absence of alarm symptoms in those aged <55 years:
Consider life changes
- Achieve and maintain healthy weight, avoid food triggers, avoid smoking, reduce caffeine intake, modify alcohol intake, avoid eating or drinking for 3hr before bed. Elevating the head of the bed with 4-6inch wooden blocks can help nocturnal reflux
Trial of alginates as required
Treat with full dose PPI (omeprazole 20mg-40mg od or equivalent) for 4 weeks
- If symptoms recur offer ongoing PPI therapy but step-down treatment to lowest effective dose
- Discuss use of “as required” treatment to encourage self- management of symptoms
- Offer an H2RA (Famotidine 20-40mg OD if inadequate response to PPI (this can be added in at bedtime in addition to PPI therapy if required)
- Secondary Care would consider using a prokinetic such as Metoclopramide 10mg TID or Domperidone 10mg TID for 4-8 weeks if inadequate response to PPI and no contra-indications, however this is unlicensed use and is not listed on the formulary for this indication. Referrers can use SCI Gateway to seek Specialist advice however, if they think this would be an option that would be helpful for a patient.
- Offer annual review to assess symptom control and reduce or withdraw treatment if possible
Special considerations
Previous oesophageal stricture dilatation
- remain on long term full dose PPI
Endoscopically diagnosed severe oesophagitis
- offer full dose PPI for 8 weeks
- if no healing consider
- High dose PPI (eg omeprazole 40mg once daily or BD)
- Switch to another PPI at full dose or high dose (in relative terms, pantoprazole is the ‘weakest’ PPI and Esomeprazole and Rabeprazole are the most potent, compared to Omeprazole) (see Resources and Links section for more info on relative PPI potencies)
- Offer long term maintenance full dose PPI
- Switch to another PPI at full or high dose if initial PPI fails to control symptoms













