Benign Sensory Symptoms that usually don’t require a neurological outpatient consultation
Dept Clinical Neurosciences, NHS Lothian. Feb 2020
Please note this is only designed as a brief summary of management.
Sensory symptoms are really common in the general population and most of the time patients don’t need a neurological consultation to deal with them. Neurology textbooks and teaching cover this area poorly, usually frightening doctors and patients with rare causes while ignoring the common ones.
This factsheet has been written to aid triage for neurology patients in NHS Lothian and to supplement letters of advice to primary care.
Are the symptoms intermittent?
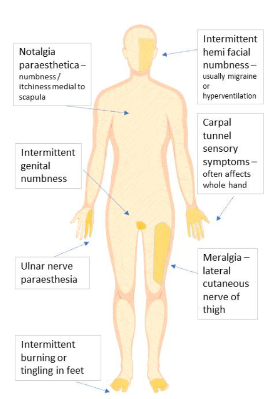
If symptoms come and go, then they are likely to be benign. Paraesthesia related to peripheral neuropathy is usually persistent (although variable) and if related to MS tends to worsen over a few days, plateau for several weeks before improving – and rarely in the distributions shown in this diagram.
In particular, if symptoms are lasting seconds or minutes then you can be really robust about having a ‘wait and see’ policy
Are they related to posture or time of day?
Hand symptoms occurring at night or in the morning are usually carpal tunnel or ulnar compression, regardless of the distribution (which often doesn’t follow textbooks). Tingling or burning in the feet mostly at night is common as part of restless legs syndrome. Meralgia may be worse after driving or with tight clothing
Facial numbness – Intermittent facial numbness is common with migraine, also in hyperventilation (where there may be perioral or tongue numbness also)
Notalgia Paraesthetica – describes an area of paraesthesia, which is sometimes itchy, in the medial scapula (where you can’t itch). It is benign but annoying and there is no investigation or treatment required
Carpal tunnel and Ulnar sensory symptoms – are common in the population. Half of our neurology trainees experience intermittent ulnar nerve sensory symptoms. Advise a wrist splint to be worn at night for 12 weeks in suspected carpal tunnel syndrome. Advise avoid leaning on elbows, prolonged elbow flexion, especially at night for ulnar nerve symptoms.
Patients with sensory symptoms only should usually be managed conservatively
Intermittent genital numbness – is nearly always benign, and commonly goes with chronic pelvic pain. Think about cauda equina/neurosurgical referral if there is clear sphincter dysfunction and/or sciatica or leg weakness.
Meralgia paraesthetica – is really common especially as the population becomes more obese. The patient will characteristically be able to draw an area with their finger around their anterolateral thigh which is numb or paraesthetic. The management is explanation, weight loss where appropriate and avoiding tight clothes in the inguinal region
Intermittent sensory disturbance in toes or burning in feet – If sensory disturbance is only in the toes, we find that we hardly ever make a diagnosis in neurology .Watch and wait. Similarly, patients with burning sensations in their feet but normal ankle jerks and no clear sensory disturbance rarely require neurological assessment.
Jon Stone and Richard Davenport, Consultant Neurologists, NHS Lothian
M.A & J.S. 05-12-22













